White Paper: Understanding Medicare Advantage Payment & Policy Recommendations 1
I. Overview
The rates paid to Medicare Advantage health plans are
determined annually through a bidding system that
is largely based on spending patterns in Traditional
Fee-For-Service (FFS) Medicare. It is imperative that
payments to Medicare Advantage health plans are
accurate, adequate and stable to allow them to provide
the necessary care to their enrollees, and to continue
to innovate in new care models and service oerings.
This White Paper provides an in-depth explanation of
the Medicare Advantage payment system, discusses
current challenges and limitations of the payment
system, and proposes several policy recommendations
to ensure consistent and stable payments in Medicare
Advantage.
Understanding Medicare Advantage
Payment & Policy Recommendations
WHITE PAPER SEPTEMBER 2018
TABLE OF CONTENTS:
I. Overview
II. Background on Medicare
Advantage
a. General Overview
b. Rate & Policy Updates:
Annual Rate Notice and
Call Letter
c. Beneficiary Enrollment
& Access
d. Types of Medicare
Advantage Plans
e. Overview of Medicare
Advantage Quality Star
Rating System
f. Medicare Advantage
& Traditional Fee-for-
Service (FFS) Medicare
III. Components of Medicare
Advantage
a. Base Rate
b. Risk Adjustment
c. Premiums
d. Rebates
e. Timeline of Key
Payment Policy
Milestones
IV. Current Challenges &
Policy Recommendations
BMA POLICY RECOMMENDATIONS TO ENSURE
PAYMENT CONSISTENCY AND STABLITY:
1. Reduce frequency of major payment policy
changes;
2. Improve the risk adjustment model and process;
3. Improve the accuracy of the benchmark
calculation; and
4. Reward quality by eliminating the benchmark
cap for plans with 4+ stars.
White Paper: Understanding Medicare Advantage Payment & Policy Recommendations 2
II. Background
A. General Overview
Medicare Advantage, also called Part C, is an option within Medicare that allows Medicare-
eligible seniors and beneficiaries with disabilities to receive their benefits through a private
plan of their choice, instead of receiving coverage through Traditional Fee-For-Service
(FFS) Medicare. Medicare Advantage plans are approved and regulated by the Centers for
Medicare & Medicaid Services (CMS). The Federal government, through CMS, pays Medicare
Advantage plans a fixed (or capitated) monthly amount per beneficiary to provide health
benefits to an enrolled individual. Medicare Advantage plans provide all Medicare Part A
and Part B services, excluding hospice. Plans have the option to oer prescription drug
coverage under Medicare Part D, which is funded through a separate bidding and payment
system.
B. Rate & Policy Updates: Annual Rate Notice and Call Letter
Medicare Advantage payment methodology and rates, as well as other policies governing
the Medicare Advantage program, are modified and updated each year. The Social Security
Act requires the Secretary of Health and Human Services to make an annual announcement,
called the Rate Notice and Call Letter, of these changes no later than the second Monday in
April before the calendar year in which the changes will be made.
1
The Social Security Act
further requires the Secretary to publish an Advance Notice and Draft Call Letter at least
60 days before publication of the Final Rate Notice and Call Letter, providing stakeholders
an opportunity to comment on proposed changes to the Medicare Advantage program. In
addition, the Secretary also issues an Early Preview of the Rate Notice in late November or
early December before the Advance Notice.
C. Beneficiary Enrollment & Access
The Centers for Medicare and Medicaid
Services (CMS) reports that 20 million
beneficiaries – or more than a third of the more
than 59 million eligible Medicare beneficiaries
– are enrolled in Medicare Advantage in 2018,
more than double the 9.7 million that were
enrolled in 2008.
2
The Congressional Budget
Oce estimates that Medicare Advantage
enrollment will grow to more than 30 million
individuals over the next 10 years.
3
While enrollment in Medicare Advantage
continues to grow, substantial geographic variation in enrollment exists. Medicare
Advantage enrollment rates at the state level range from a low of 2% in North Dakota to a
BMA’s Medicare Advantage
Enrollment Map provides
Medicare Advantage
enrollment information
at the county and
Congressional district level.

White Paper: Understanding Medicare Advantage Payment & Policy Recommendations 3
high of 44% in Oregon.
4
This variation is due to many factors, including long-term insurance
market factors in states as well as specific characteristics of each state – for example,
low penetration rates due to a state being rural and sparsely populated (e.g. Vermont,
Wyoming), high penetration rates due to a concentration of retirees (e.g. Florida, Arizona),
or a large number of hospital-owned plans (e.g. Minnesota, Oregon).
Beneficiary access to Medicare Advantage is strong. In 2018, Medicare Advantage included
2,317 individual plan options.
5
In total, 99% of all Medicare beneficiaries have access to a
Medicare Advantage plan and most beneficiaries have multiple plans to choose from in their
area.
6
A recent analysis found that 90% of Medicare Advantage beneficiaries have a choice
of at least five Medicare Advantage plan options, 71% have at least 10 plans options, and
55% have at least 15 plan options.
7
More than 80% of all beneficiaries have access to at least
one zero premium plan, and 40% of beneficiaries are enrolled in a zero premium plan.
D. Types of Medicare Advantage Plans
Medicare Advantage plans oer coordinated care, typically organized around a network of
health care providers that works to manage enrollees’ care. Each Medicare Advantage plan
establishes its own network of providers, subject to legislative and regulatory requirements
that determine the number and type of providers that must be included in a plan’s service
area.
The types of Medicare Advantage plans available to beneficiaries are:
1. Health Maintenance Organizations (HMOs): HMOs often require members to choose a
primary care physician to coordinate their care and utilize network providers or pay the
full cost of care received outside the network. Generally, HMOs require a referral from
a primary care physician to see a specialist. In 2018, more than 60% of enrollees are in
HMOs.
8
2. Preferred Provider Organizations (PPOs): PPOs are similar to HMOs, but they may not
require members to select a primary care physician, and they often do not require a
referral to see a specialist. They may oer coverage for health care services received
outside the network, but typically require members to pay a larger portion of the cost of
out-of-network care. PPOs may be local (county-specific) or regional (span two or more
states). In 2018, approximately 34% of enrollees are in PPOs.
9
3. Private Fee-For-Service (PFFS): PFFS plans allow enrollees to see any Medicare-eligible
health care provider who accepts payment from that plan; however, they may oer
members financial incentives to use certain providers. Just 1% of Medicare Advantage
enrollees selected a (PFFS) plan. In 2018, less than 1% of enrollees are in PFFS plans.
10
4. Special Needs Plans (SNPs): SNPs are a type of Medicare Advantage plan tailored to
serve frail, disabled, and chronically-ill beneficiaries. There are SNPs tailored to enrollees
who are dually eligible for both Medicare and Medicaid, those who have a severe or
disabling chronic condition, or those who live in a nursing home or who require skilled

White Paper: Understanding Medicare Advantage Payment & Policy Recommendations 4
nursing care at home. In 2018, approximately 13% of Medicare Advantage members are
enrolled in SNPs.
11
5. Employer Group Waiver Plans (EGWPs): EGWPs are a type of Medicare Advantage plan
oered by an employer to its retiree population. In 2018, approximately 20% of Medicare
Advantage members are enrolled in EGWPs.
12
E. Overview of Medicare Advantage Quality Star Rating System
Medicare Advantage plans are awarded a star rating between one and five based on
performance on certain quality measures in the Medicare Advantage Quality Star Rating
System. The Star Rating System plays a critical role in ensuring public accountability and
enhancing consumer choice by providing quality information on plans. Star ratings foster
competition between plans to improve quality and may lead to quality-based financial
incentives for some plans and providers. In 2018, 73% of Medicare Advantage enrollees are
enrolled in high-performing four- or five-star plans, almost quadruple the percent of those
enrolled in high-performing plans in 2009.
F. Medicare Advantage & Traditional Fee-for-Service (FFS) Medicare
The financial framework in Medicare Advantage supports care delivery that focuses on
care management, integrated care models, and early interventions. Because Medicare
Advantage plans receive a capitated (fixed) monthly payment per beneficiary to provide
health benefits to enrollees, the plan is at-risk if costs for an enrollee exceed the capitated
payment (plus enrollee cost-sharing). At the same time, if costs are less than the capitated
payment (plus enrollee cost-sharing), plans retain the savings.
The capitated payment structure aligns plan financial incentives with patient health
outcomes, motivating Medicare Advantage plans to oer care coordination as well as
preventive services, early interventions and other services that help enrollees stay healthy
and avoid unnecessary, costly health care services, such as emergency room visits and
hospital admissions. In addition, as described in detail below, if a plan receives rebates from
CMS, it must use those funds to reduce enrollee out-of-pocket costs or to provide additional
supplemental benefits, such as dental or vision coverage.
Payments to Medicare Advantage plans are based on FFS Medicare. As detailed below,
Medicare Advantage payments are largely based on average FFS Medicare spending in
individual counties across the country.
White Paper: Understanding Medicare Advantage Payment & Policy Recommendations 5
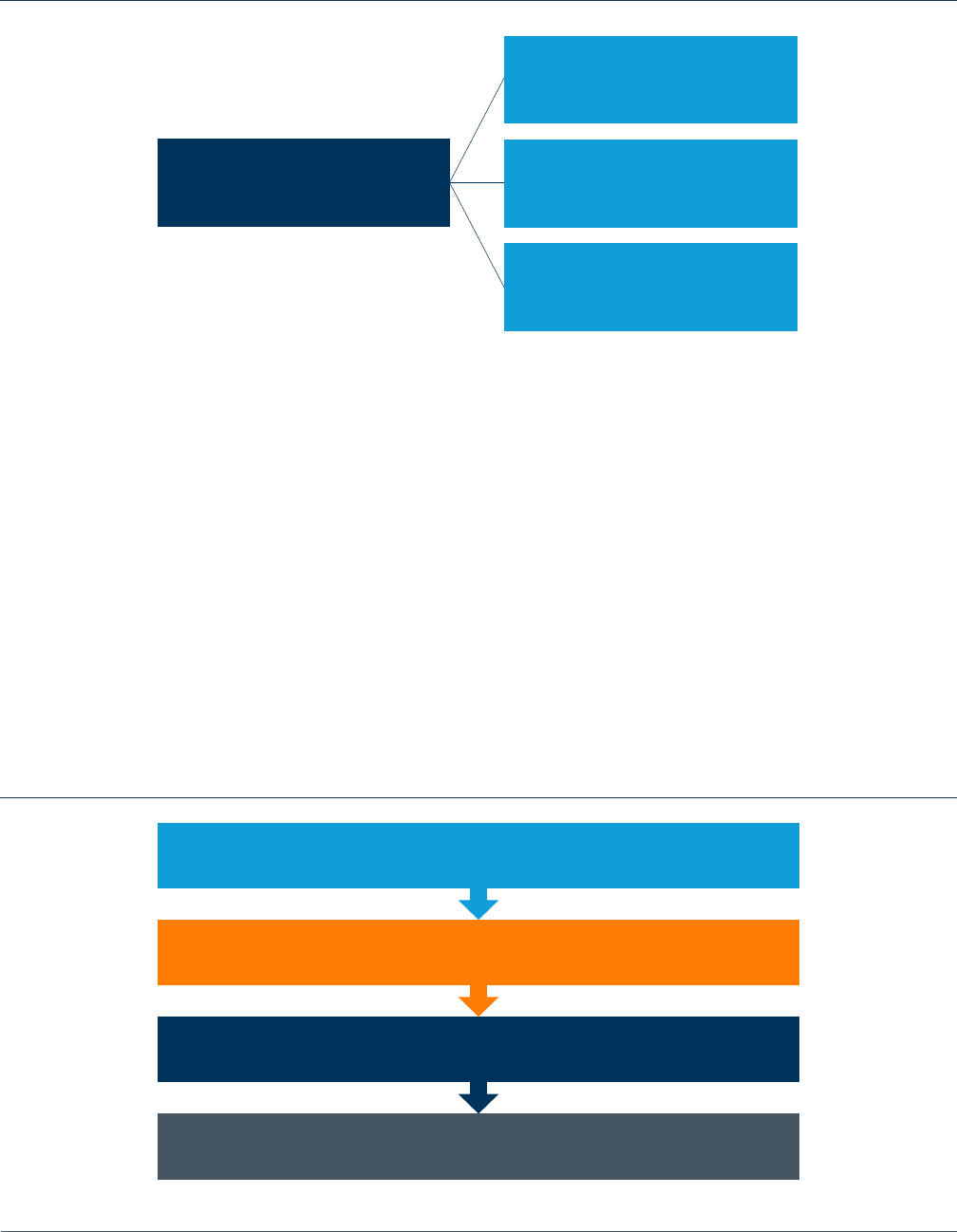
III. Components of Medicare Advantage Payment
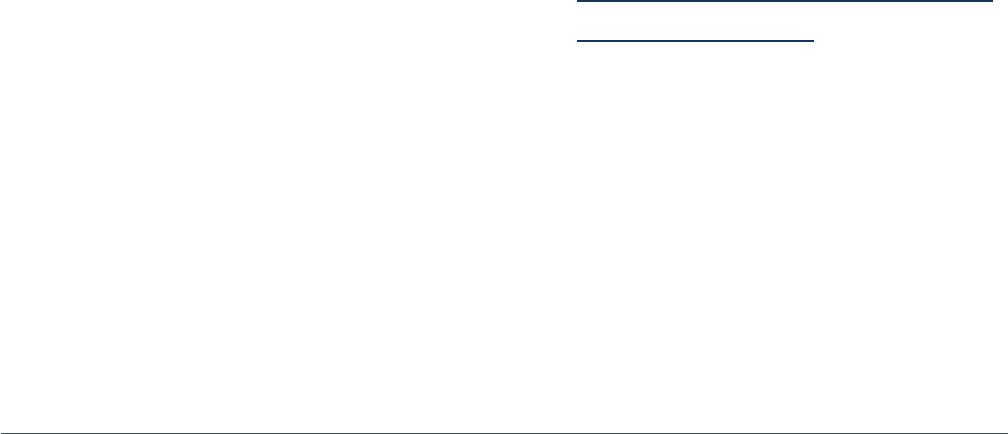
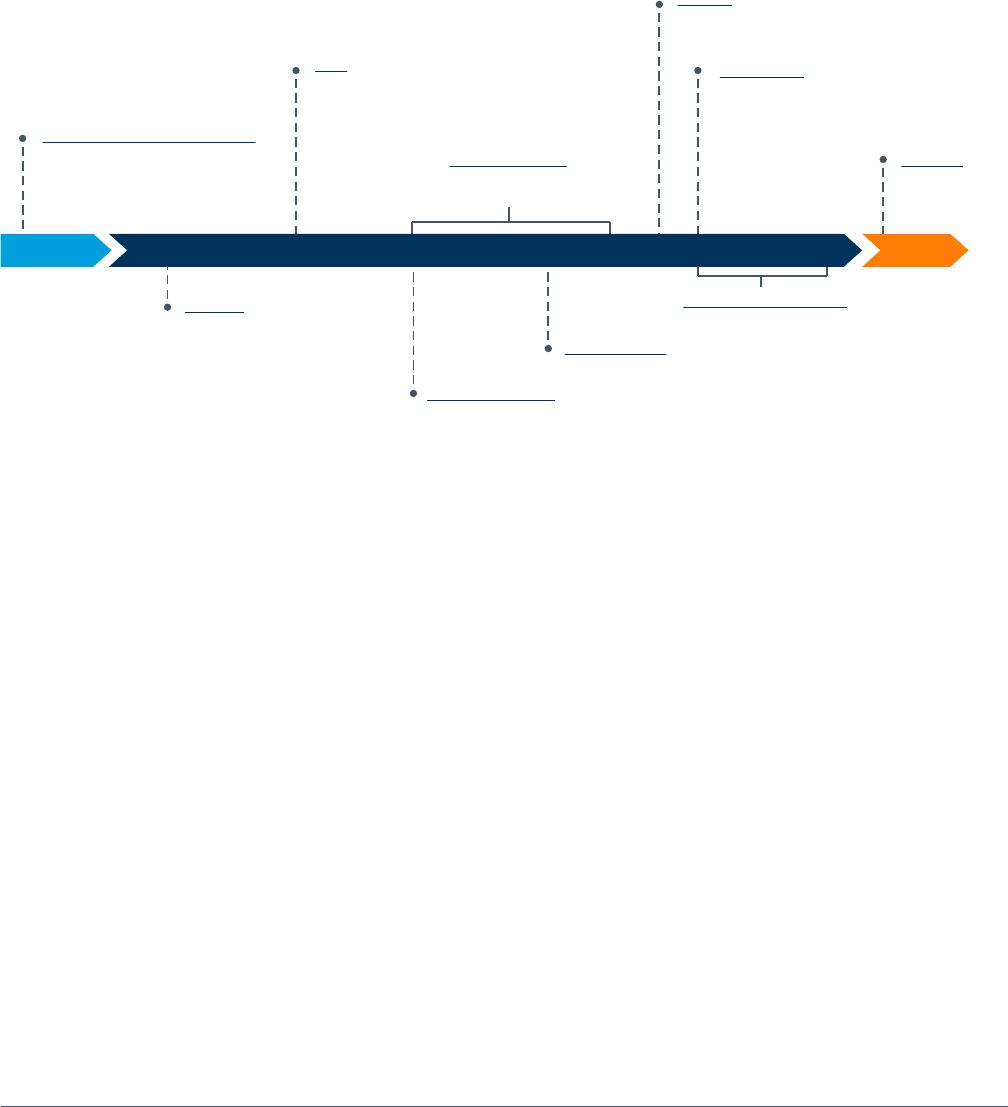
There are four key components that together determine what Medicare Advantage health
plans are paid to provide care for their enrollees:
• Base rate. The base rate is the lesser of the plan’s bid or the benchmark rate. If a plan’s
bid is below the benchmark, then the base rate equals the plan’s bid. If a plan’s bid is
above the benchmark, then the base rate equals the benchmark.
• Risk adjustment. The base rate for a particular enrollee is then adjusted to reflect that
enrollee’s risk score.
• Premiums. Plans that bid below the benchmark may not charge any enrollee premium.
Plans that bid above the benchmark charge a premium that is equal to the dierence
between the bid and the benchmark.
• Rebates. Plans that bid below the benchmark receive a rebate equal to a percentage of
the dierence between the benchmark and the bid.
Each of these components are described in greater detail below.
FIGURE 1: SUMMARY OF MEDICARE ADVANTAGE PAYMENT
Base Rate
=
Standard
Bid
Risk Adjustment
Plan Bid
Below
Benchmark
Plan Bid
Not Below
Benchmark
CMS-HCC CMS-HCC
Enrollee
Basic Premium
Always 0
Payment
to Plan
Payment
to Plan
Rebate = 0.5 to 0.7
varies by plan star rating
x
risk adjusted
benchmark-actual bid
Patient characteristics:
Diagnoses, Sex, Working aged status, Age,
Medicaid status, Disabled status
Adjustment (if any) to
CMS payment for risk
model factors of individual
enrollees to maintain fixed
enrollee premium
Enrollee
Basic Premium
Equal to the
Dierence between
the bid and the
benchmark
Base
Rate
CMS-
HCC
Risk
Score
Base Rate
=
Benchmark
x
=
=
+
+
–
+
+
ŧ
ŧ
ŧ
ŧ
ŧ
ŧ
Source: MedPAC. “Medicare Advantage Payment System Basics.” October 2016. Available at: http://medpac.gov/docs/
default-source/payment-basics/medpac_payment_basics_16_ma_final.pdf?sfvrsn=0
White Paper: Understanding Medicare Advantage Payment & Policy Recommendations 6
A. Base Rate
The first component of the payment to a Medicare Advantage plan is the base rate. The
base rate is determined by the relationship between the county-level benchmark and the
plan bid. First, CMS determines the average FFS Medicare spending in each county, which,
following adjustments for geography and demographics, becomes the benchmark. Second,
Medicare Advantage plans bid to provide coverage in a county. Finally, CMS compares each
plan’s bid to the benchmark. The base rate is the lower of the plan’s bid or the benchmark.
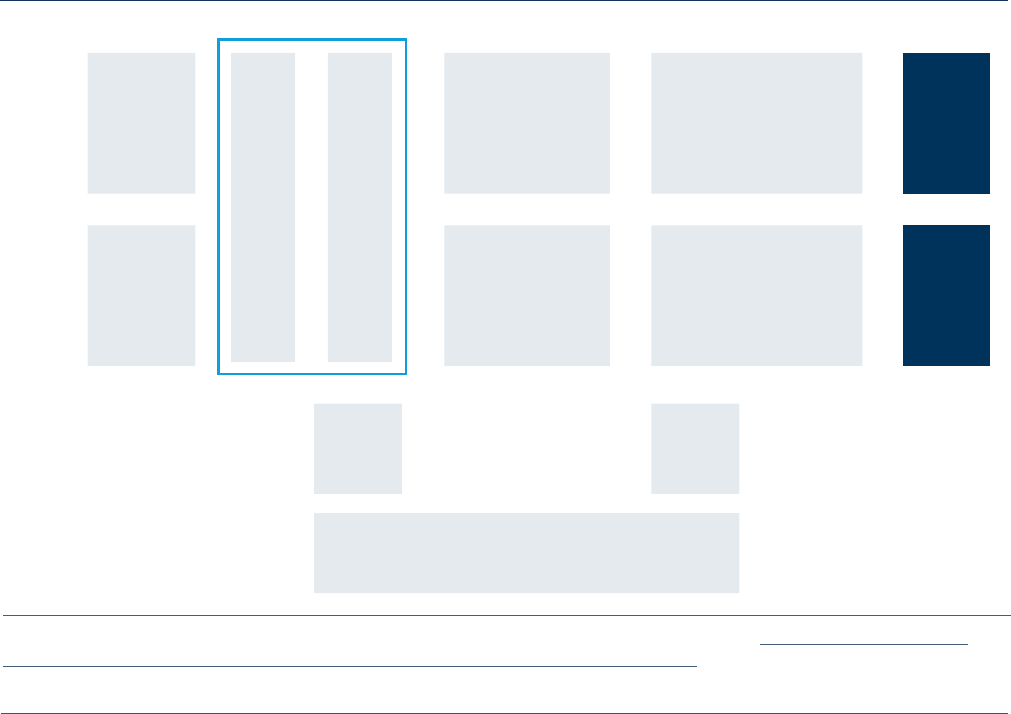
FIGURE 2: HYPOTHETICAL BID AND BENCHMARK SCENARIOS
1. Benchmarks
i. Benchmarks Defined
Benchmarks are the targets against which plans bid to provide coverage of Medicare Part
A and Part B services. A separate benchmark is calculated for each county in the United
States and is set as a percentage of average FFS Medicare spending per beneficiary. This
means that Medicare Advantage benchmark levels in each county are based on the practice
patterns of physicians and other providers who bill FFS Medicare.
For payment purposes, Medicare Advantage plans fall under one of two categories: local
plans or regional plans. Local plans may be any type of plan (HMO, PPO, PFFS) and may
serve beneficiaries living in one or more counties. Regional plans must be PPOs and serve
all of one of the 26 regions established by CMS.
Establishing the benchmarks for both local and regional plans requires a determination
of per capita FFS Medicare spending for each county. To make this determination, the
Secretary first projects the national estimated FFS Medicare per capita costs for the
following year ($848.21 per month for 2018).
13
This amount is then multiplied by a county-
specific geographic index, which is based on a five-year rolling average of FFS Medicare
Benchmark = $1,000
Plan Bids above Benchmark
Plan bid=$1,100
Plan payment from CMS = $1,000
Plan Bids above Benchmark
Plan bid=$1,100
Plan payment from CMS = $1,000
Plans that receive 4 or 5
stars are eligible to receive
a higher rebate percentage
Rebate amount = $50
Beneficiary preimium for
Part A/B services = $100
CMS savings = $50
White Paper: Understanding Medicare Advantage Payment & Policy Recommendations 7
spending in the county, weighted for enrollment and average risk scores, to yield the per
capita FFS Medicare spending amount for each county.
ii. County-Level Benchmark Calculation: Local Plans
To determine the county-level benchmarks for local plans, the per capita FFS Medicare
spending amount is adjusted based on the county’s historical costs relative to the rest of
the nation. Counties with the lowest FFS Medicare spending receive the highest percentage
of per capita FFS Medicare spending as their benchmark. These percentage adjustments
were established by the Aordable Care Act as follows:
Highest-cost quartile 95% of FFS costs
Second-highest cost quartile 100% of FFS costs
Third-highest cost quartile 107.5% of FFS costs
Lowest-cost quartile 115% of FFS costs
For a local Medicare Advantage plan that operates in more than one county, an average
benchmark is calculated across the counties in which the plan operates, weighted by
enrollment.
iii. County-Level Benchmark Calculation: Regional Plans
The process for calculating benchmarks for regional plans, which must serve all of at
least one of the 26 regions established by CMS, is a bit more complex. These regional
benchmarks are a weighted average of:
• the average county-level benchmark (described above), weighted by the number of
Medicare beneficiaries in each county and the national percentage of beneficiaries
in FFS Medicare, and
• the average plan bid, weighted by each plan’s projected enrollment and the national
percentage of beneficiaries in Medicare Advantage.
14
iv. Quality Adjustments to Benchmarks
Benchmarks for both local and regional Medicare Advantage plans are also adjusted based
on plan quality. Plans with a 4, 4.5, or 5-star quality rating from CMS receive an increase in
their benchmark (5% in 2018).
15
In addition, these benchmark quality adjustments may be
doubled for high-quality plans in certain qualifying counties (urban areas with FFS Medicare
spending below the national average and historically high rates of enrollment in Medicare
Advantage).

White Paper: Understanding Medicare Advantage Payment & Policy Recommendations 8
v. Benchmark Caps
In many counties across the country, benchmarks (including quality adjustments) are
capped at their pre-ACA levels. In 2017, benchmarks in half of counties across the country
were constrained in some way by the benchmark cap, meaning plans with 4 or more stars
received a benchmark quality bonus less than the statutory 5% or received no quality bonus
at all.
16
In 2016, more than 2 million Medicare beneficiaries were enrolled in 4-star plans but
denied enhanced benefits, including reduced cost-sharing, because of the benchmark cap.
2. Plan Bids
With benchmarks determined, the next step in the payment process is the submission of
plan bids. Medicare Advantage plans submit bids reflecting the plan’s estimated cost of
providing all Medicare Part A and Part B services to a beneficiary with “average” health,
with the exception of hospice. Bids include the estimated costs of medical services as well
as administrative expenses and profit. However, plan administrative expenses and profit may
not exceed 15% of total plan revenue, ensuring that 85% of revenue is dedicated to member
benefits. Plans that do not meet this minimum medical loss ratio (MLR) requirement must
refund CMS the dierence between their MLR and 85%.
Medicare Advantage plans that wish to oer Part D prescription drug benefits submit a
separate bid for the Part D portion of coverage. Payment for Part D-covered services is
calculated separately, in the same manner as it is for plans oering standalone prescription
drug coverage.
3. Calculation of the Base Rate
A Medicare Advantage plan’s base rate is determined by comparing the plan’s bid and the
benchmark. If the plan’s bid is below the benchmark, the bid becomes the plan’s base rate.
If the plan’s bid is at or above the benchmark, then the benchmark becomes the plan’s
base rate, and the dierence is returned to enrollees in the form of reduced cost sharing
obligations or enhanced benefits.
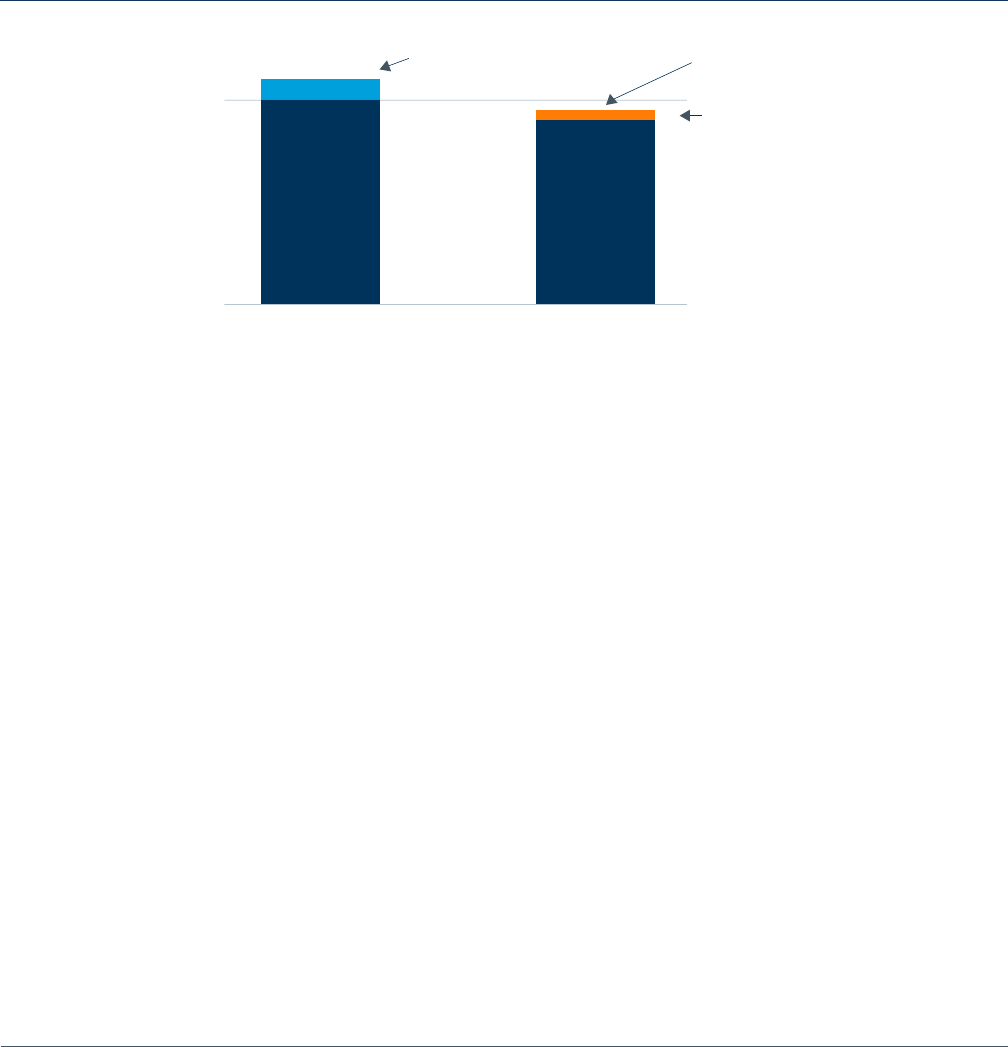
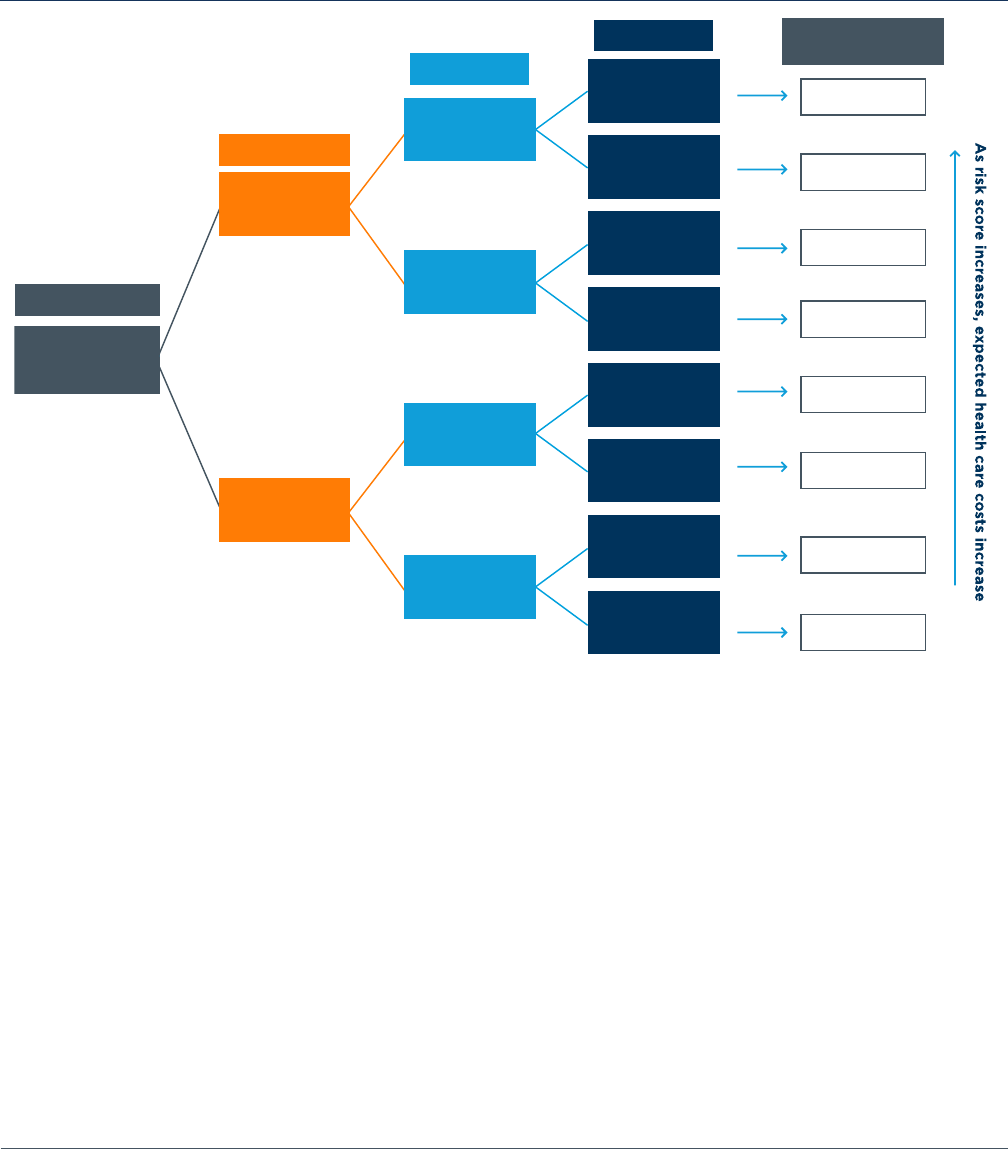
B. Risk Adjustment
After the base rate is determined, CMS uses a system called “risk adjustment” to modify
a plan’s base rate to reflect the health status of each enrollee. This ensures capitated
payments made to Medicare Advantage plans reflect the expected cost of providing health
care to each beneficiary.
17
A risk score of 1.0 implies that the person’s expected costs are
equal to the costs of a beneficiary of average health. An enrollee with a risk score of 2.0 is
expected to cost twice as much as the average, whereas an enrollee with a risk score of 0.5
is expected to cost 50 percent less than average (see Figure 3).
White Paper: Understanding Medicare Advantage Payment & Policy Recommendations 9
FIGURE 3: INDIVIDUAL RISK SCORES
Since 2004, CMS has used the Hierarchical Condition Categories (CMS-HCC) model to
risk adjust Medicare Advantage base rates. The CMS-HCC model uses diagnoses from
inpatient, outpatient, and physician encounters to provide a comprehensive accounting
for the full range of patient spending. To generate a risk score, CMS first groups all
International Classification of Disease, Tenth Edition (ICD-10) codes into diagnostic
groups called DxGroups. These groups include diagnosis codes that cover similar medical
conditions. Second, CMS combines the DxGroups into Condition Categories (CCs), which
groups enrollees based on similar clinical profiles and expected costs. Third, CMS imposes
hierarchies on the model by dropping a less severe manifestation of the disease if a more
severe manifestation is present. Finally, once the hierarchies are applied, CMS publishes the
list of categories, or Hierarchical Condition Categories (HCCs), as part of the annual rate
announcement, typically located in a table in a supplemental attachment. This process is
illustrated in Figure 4 below.
FIGURE 4: MEDICARE ADVANTAGE RISK ADJUSTMENT PROCESS BEGINS BY GROUPING DISEASES AND ASSIGNING HCCS
Group ICD-10 codes into DxGroups that represent a medical condition
Combine DxGroups into Condition Categories that are similar clinically
and in terms of cost
Impose hierarchies so that person only is coded with most severe
manifestation of disease
Select HCCs to include for payment
Risk Score = 0.5
Expected costs are 50% lower than
Costs for the average beneficiary
Risk Score = 1.0
Expected costs are equal to
Costs for the average beneficiary
Individual Risk Scores Assess
Relative Health Care Costs
Risk Score = 2.0
Expected costs are two times higher
Than costs for the average beneficiary
White Paper: Understanding Medicare Advantage Payment & Policy Recommendations 10
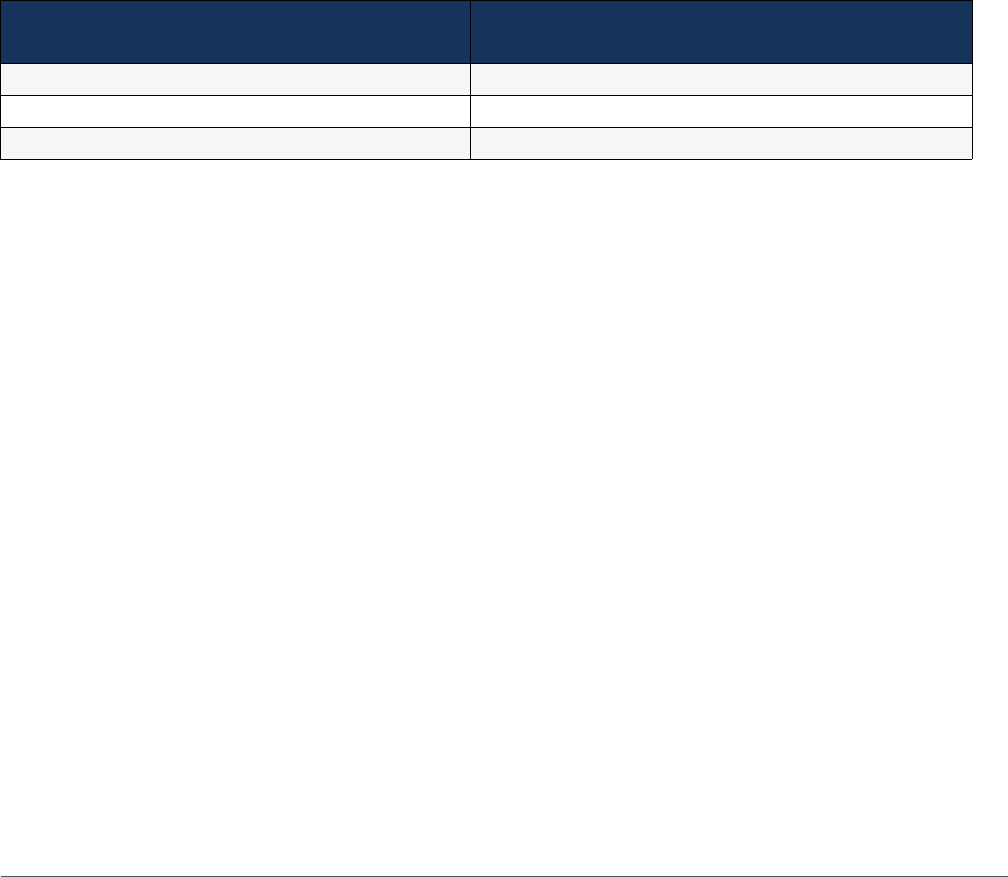
Each HCC has an associated coecient (or weight). The coecients for each HCC are
added, along with those for age and gender, to determine the risk score, as shown in Figure
5.
18
CMS estimates the costs associated with dierent risk scores based on FFS Medicare
spending and utilization data.
FIGURE 5: MEDICARE ADVANTAGE RISK ADJUSTMENT EXAMPLE
Because CMS uses FFS Medicare data to calculate payments to Medicare Advantage plans,
it also must adjust those payments to account for coding pattern dierences that exist
between Medicare Advantage and FFS Medicare. These coding dierences arise from
structural, payment, and care model dierences between FFS Medicare and Medicare
Advantage. For instance, because CMS uses diagnosis codes submitted by providers to
risk-adjust plan payments, Medicare Advantage plans have an incentive to ensure accuracy
in diagnosis codes both to ensure adequate payment to meet beneficiary needs and to
identify at-risk individuals for early intervention and care management. FFS Medicare does
not require the same specificity in diagnosis coding because payments to providers rely
on procedure codes. To account for this dierence, Congress mandated an annual coding
intensity adjustment in 2010 and subsequent years which requires CMS to reduce Medicare
Advantage risk scores by a uniform, pre-determined factor every year. As of 2018, the
reduction is 5.91% annually. CMS has the statutory authority to increase the annual coding
intensity adjustment but, to date, has not used that authority.
Age and Gender
HCC 111
HCC 86
HCC 88
1.149
1.009
0.916
0.776
0.821
0.681
0.588
0.448
Normalized
Risk Score
Female beneficiary,
age75
(0.448)
COPD
(0.328)
Acute Myocardial
Infarction
(0.233)
Angina Pectoris
(0.140)
Angina Pectoris
(0.140)
Angina Pectoris
(0.140)
Angina Pectoris
(0.140)
No Angina Pectoris
No Angina Pectoris
No Angina Pectoris
No Angina Pectoris
No Acute
Myocardial
Infarction
No Acute
Myocardial
Infarction
Acute Myocardial
Infarction
(0.233)
No COPD
White Paper: Understanding Medicare Advantage Payment & Policy Recommendations 11
C. Premiums
The third component of payment to a Medicare Advantage plan is the enrollee premium.
Depending on how a plan’s bid compares to the benchmark, the plan may charge enrollees
a monthly premium. If a plan bids above the benchmark, then the enrollee pays a premium
equal to the dierence between the bid and the benchmark. If a plan bids below the
benchmark, there is no member premium.
D. Rebates
The fourth and final component of the payment to a Medicare Advantage plan is the rebate.
All plans that bid below the benchmark receive a percentage of the dierence between the
bid and benchmark as a rebate, ranging from 50% to 70% of the dierence between the bid
and the benchmark. The amount of the rebate paid to the plan is determined by the plan’s
quality star rating; plans with higher star ratings receive Quality Bonus Payments (QBPs) in
the form of a higher percentage of the dierence as a rebate, as follows:
Plan Quality Star Rating
Percent of Bid-Benchmark Dierence
Paid to Plan as a Rebate
3 Stars or fewer 50%
3.5 - 4 Stars 65%
4.5 - 5 Stars 70%
Plans are required to use rebates and QBPs to provide supplemental benefits, such as
hearing, dental or vision, to reduce beneficiary cost-sharing, or to provide innovations in
care delivery, such as telemedicine or home care. The combination of zero premiums and
additional benefits incentivizes Medicare beneficiaries to select high-quality, lower-cost
Medicare Advantage plans.
White Paper: Understanding Medicare Advantage Payment & Policy Recommendations 12
E. Timeline of Annual Payment Policy Milestones
Benchmark development, bid submission, and determination of each plan’s payment is a
lengthy process with many steps, identified below.
19
November (of the previous year)
CMS releases an early preview of
rates for the following plan
payment year
February
CMS publishes Advance Notice
and Draft Call Letter with a
30-day comment period
April
CMS publishes Final Rate Notice
and Call Letter for the following
plan payment year
June - September
CMS reviews and approves bid
data; Actuarial certifications due
June (first Monday)
Medicare Advantage
plans submit bids
Mid-October
Medicare Advantage
plan quality star ratings
for following payment
year announced
October 15 - December 7
Open Enrollment
Mid-September
Contracts fully executed
October
Medicare Advantage plans
may begin marketing
January 1
Plan Benefit
Period Begins

White Paper: Understanding Medicare Advantage Payment & Policy Recommendations 13
IV. Current Challenges & Policy Recommendations
There are challenges in the Medicare Advantage payment system that potentially
undermine the consistency and stability of payment and may impact the resources
available to care for beneficiaries and to invest and innovate in new models to improve
care delivery and contain costs. To address these challenges, BMA makes the following
recommendations:
1. Reduce frequency of major payment policy changes
Challenge. As noted above, CMS issues an Advance Notice of Methodological Changes
and Draft Call Letter each year in February and finalizes these proposed changes each
April. Through this annual rate setting process, CMS may change any or every element
of Medicare Advantage payment rates, including changes to the risk adjustment model,
Star Ratings system, and other factors that significantly influence payment rates. Plans
operating in this unpredictable and unstable rate setting environment must prepare for
unstable funding and unforeseen rate cuts, which may not be aligned with multi-year
contracts between plans and multiple providers, including value-based contracts. This
unpredictability impacts eorts to make investments in innovation and care delivery
programs that better meet the needs of Medicare Advantage enrollees and may negatively
impact beneficiary cost sharing reductions or enhanced benefits.
Policy Recommendation. To bring some stability to the rate setting process, BMA
encourages CMS to consider a multi-year process for Medicare Advantage payment policy
changes. Using a multi-year process will help streamline and alleviate unnecessary burdens
in the regulatory process, provide predictability to Medicare Advantage plans so they may
invest in innovation and care improvements, encourage multi-year value-based contracting
that includes multi-year goals regarding risk-assumption by the provider, and reduce
administrative burdens on health care providers. A multi-year policy change process would
also bring stability to plans’ community partners that are asked to build workforce and
administrative infrastructure. In a multi-year policy setting process, CMS would be able to
spread policy changes over a multi-year cycle while continuing to make annual rate updates
required by statute.
BMA POLICY RECOMMENDATIONS TO ENSURE PAYMENT CONSISTENCY AND STABLITY:
1. Reduce frequency of major payment policy changes;
2. Improve the risk adjustment model and process;
3. Improve the accuracy of the benchmark calculation; and
4. Reward quality by lifting the benchmark cap.

White Paper: Understanding Medicare Advantage Payment & Policy Recommendations 14
2. Improve the risk adjustment model and process
Challenge. CMS has changed the risk adjustment model over the past several years in an
eort to improve payment accuracy.
20
However, challenges remain both in terms of the
model itself and the process for making further changes. While changes in the model
to improve accuracy and adequacy of payment to meet beneficiary needs are essential,
the stability of the model is also critical. Any changes to the risk adjustment model are
dicult for stakeholders, including clinicians, to understand, assess, and implement. These
challenges are amplified when stakeholders have limited information regarding the impacts,
consequences, or concerns about both the current model and proposed changes.
In addition to challenges with the coding intensity adjustment, described above, several
structural challenges exist within the risk adjustment model. First, CMS has found that the
current risk model underpays Medicare Advantage plans for coverage provided to dual-
eligible beneficiaries, who are among the most high-need, high-cost, high-risk enrollees
and require more specialized care and management. Second, stakeholders continue to have
concerns regarding the risk model’s ability to accurately predict costs for individuals living
with multiple chronic conditions.
Third, stakeholders have raised serious concerns about the transition to the Encounter
Data System (EDS) as the single source of enrollee diagnosis data used as the basis for risk
scores. These concerns were recently echoed by the Government Accountability Oce,
which concluded that limited progress has been made to validate the EDS, potentially
resulting in inaccurate risk scores.
21
CMS is transitioning the system used to gather diagnosis
codes and is currently using a blended version of two dierent systems. Under the current
system, Medicare Advantage plans filter diagnosis codes and submit them to CMS, where
the files are reviewed and audited for accuracy. With the newer EDS, Medicare Advantage
plans submit all unfiltered data directly to CMS, which then applies its own filtering logic to
extract diagnosis codes.
Policy Recommendations.
1
A well-functioning risk adjustment program must adequately
pay plans that enroll high-cost individuals and manage their care eectively. With millions
of baby boomers aging into Medicare, it is essential that risk adjustment in Medicare
Advantage provides for adequate payment to care for all beneficiaries, ensuring the long-
term sustainability and eectiveness of the program.

White Paper: Understanding Medicare Advantage Payment & Policy Recommendations 15
Briefly, BMA recommends the following:
• Maintain coding intensity adjustment at the statutory minimum level, to achieve stability
and adequacy of the prospective, capitated payment and enable plans and providers to
gather the data necessary for early intervention and care management;
• Improve risk model accuracy for individuals with multiple chronic conditions, considering
the cumulative impact of a large number of chronic conditions, the interaction between
behavioral/mental health conditions and physical health conditions, the dierences in
dual-eligible beneficiary costs given dierent eligibility pathways, and the potential for
using more than one year of data to establish risk scores;
22, 23
• Incorporate social determinants of health into the risk model as proposed and executed
by CMS and the National Quality Forum (NQF) for quality measures in the Star Rating
System. As Medicare Advantage grows and becomes increasingly complex, a better
understanding of how social determinants of health aect beneficiary costs, and
adjusting payments accordingly, will be critical;
• Validate the Encounter Data System to ensure accuracy of risk scores for Medicare
Advantage enrollees before progressing further in calculating risk scores using encounter
data; and
• Improve transparency of the risk adjustment model change process by improving the
notice and comment process, publishing and responding to all comments received, and
conducting open door forums.
3. Improve the accuracy of the benchmark calculation
Challenge. In order to measure average FFS spending to calculate county-level benchmarks,
CMS uses data for all FFS beneficiaries in a county, including those who have both Part A
and Part B, those who have only Part A, and those who have only Part B. However, in order
to enroll in a Medicare Advantage plan, beneficiaries must enroll in both Part A and Part B.
MedPAC has found that a smaller share of FFS Medicare beneficiaries are enrolled in both
Part A and Part B over the past few years.
24
MedPAC has also found that per beneficiary
spending is higher for beneficiaries enrolled in both Part A and Part B than the combined
total of average spending for all beneficiaries enrolled in Part A and all beneficiaries
enrolled in Part B. Finally, in its analysis of risk scores, MedPAC found that the average risk
score of beneficiaries enrolled in both Part A and Part B is higher than average risk scores
for all enrollees in either Part A or Part B.
Policy Recommendation. BMA supports MedPAC’s recommendation that CMS should
calculate Medicare Advantage benchmarks using FFS Medicare spending only for
beneficiaries enrolled in both Part A and Part B in order to improve accuracy in the
benchmark calculation.

White Paper: Understanding Medicare Advantage Payment & Policy Recommendations 16
4. Reward high quality by eliminating the benchmark cap for plans with
4+ stars
Challenge. The Quality Star Rating System program plays a key role in keeping Medicare
Advantage eective and innovative by incentivizing improvements in quality. Medicare
Advantage enrollees benefit from both these quality improvements and from the
requirement that plans use rebates that result from bidding below the benchmark and
quality bonuses to reduce enrollee cost-sharing or increase benefits. Under current law,
county-level benchmarks (including quality adjustments) are capped at their pre-ACA
levels.
The benchmark cap prevents plans in certain counties from receiving the bonus payments
they earn and prevents beneficiaries from receiving the full benefits of enrolling in a high-
quality plan. In 2017, benchmarks in half of counties across the country were constrained
in some way by the benchmark cap, meaning plans with 4 or more stars received a
benchmark quality bonus less than the statutory 5% or receive no quality bonus at all.
25
In
2016, more than 2 million Medicare beneficiaries were enrolled in 4-star plans but denied
enhanced benefits, including reduced cost-sharing, because of the benchmark cap.
Policy Recommendation. CMS should lift the benchmark cap for high quality, 4-star and
higher Medicare Advantage plans to ensure that all Medicare Advantage beneficiaries
receive the full benefits of enrolling in a high-quality plan.

White Paper: Understanding Medicare Advantage Payment & Policy Recommendations 17
1
42 U.S.C. Sec. 1395w-23(b). Web.
2
Centers for Medicare & Medicaid Services, “Monthly Contract and Enrollment Summary Report,” July 2017.
Web.
3
Congressional Budget Oce, “June 2017 Baseline,” June 29, 2017. Web.
4
Better Medicare Alliance, “Beneficiaries Continue to Choose Medicare Advantage,” October 2017. Web.
5
Kaiser Family Foundation, “Medicare Advantage 2018 Data Spotlight: First Look,” October 2017. Web.
6
Medicare Payment Advisory Commission, “Report to the Congress: Medicare Payment Policy,” March 2018.
Web.
7
Better Medicare Alliance, “Beneficiaries Continue to Choose Medicare Advantage,” October 2017. Web.
8
Better Medicare Alliance analysis of CMS Medicare Advantage Enrollment Data, July 2018.
9
Ibid.
10
Ibid.
11
Ibid.
12
Ibid.
13
Paulette C. Morgan, “Medicare Advantage—Proposed Benchmark Update and Other Adjustments for
CY2018: In Brief,” Congressional Research Service, February 17, 2017. Web.
14
Medicare Payment Advisory Commission, “Medicare Advantage System Payment Basics,” October 2017.
Web.
15
Paulette C. Morgan, “Medicare Advantage—Proposed Benchmark Update and Other Adjustments for
CY2018: In Brief,” Congressional Research Service, February 17, 2017. Web.
16
Paulette C. Morgan, “Medicare Advantage—Proposed Benchmark Update and Other Adjustments for
CY2018: In Brief,” Congressional Research Service, February 17, 2017. Web.
17
For further information on risk adjustment, see Better Medicare Alliance, “Medicare Advantage Risk
Adjustment: Evolution and Current Issues,” October 2017. Web.
18
Better Medicare Alliance, “Medicare Advantage Risk Adjustment: Current Issues, Evolution & Policy
Recommendations,” March 2018. Web.
19
Milliman, “Regulatory Oversight in Medicare Advantage,” June 24, 2016. Web.
20
Better Medicare Alliance, “Medicare Advantage Risk Adjustment: Current Issues, Evolution & Policy
Recommendations,” March 2018. Web.
21
United States Government Accountability Oce, Medicare Advantage: Limited Progress Made to Validate
Encounter Data Used to Ensure Proper Payments, January 2017. Web.
22
United States Senate, Committee on Finance, Bipartisan Chronic Care Working Group, Policy Options
Document, December 2015. Web.
Sources

White Paper: Understanding Medicare Advantage Payment & Policy Recommendations 18
23
Better Medicare Alliance, “Medicare Advantage Risk Adjustment: Current Issues, Evolution & Policy
Recommendations,” March 2018. Web.
24
Medicare Payment Advisory Commission, “March 2017 Report to the Congress: Medicare Payment Policy,
Chapter 13: Status report on the Medicare Advantage Program,” March 15, 2017. Web.
25
Paulette C. Morgan, “Medicare Advantage—Proposed Benchmark Update and Other Adjustments for
CY2018: In Brief,” Congressional Research Service, February 17, 2017. Web
