
STANFORD MEDICINE SEPTEMBER 2018
White Paper:
The Future of Electronic
Health Records

Introduction
Ten years ago, one doctor in 10 kept
digital records on their patients. The
other 90 percent made notes on paper
and stored them in manila folders on
shelves and in filing cabinets.
Paper records had some obvious
disadvantages. They took up space,
they were diicult to share with
other physicians, hospitals, and
insurance companies.
Patients switching doctors, hospitals,
or places of residence could not easily
bring their records with them.
In 2009, in the wake of the financial
crisis, the federal government acted
to remedy this situation. The Health
Information Technology for Economic
and Clinical Health (HITECH) Act set
aside $27 billion of federal funds
to encourage health care providers
to adopt electronic health record
(EHR) systems, and more money was
subsequently made available for training
and assistance. All told, the federal
government spent about $35 billion on
bringing the U.S. health care industry
into the electronic age. The program was
highly successful in that it made EHRs
commonplace. Today, nine in 10 doctors
have adopted them. “We have made a
colossal transformation in a relatively
short period of time,” says Lloyd Minor,
MD, Dean of Stanford Medicine. “But we
have not realized the potential benefits
of the data that exist in electronic health
records.”
Indeed, many of the benefits of EHRs
have been elusive. As implemented
today, EHRs have too many of the
drawbacks of paper records. The
promise of being able to send them
easily from one oice to the next has
been hampered by a lack of standards
and perverse incentives in the health
care marketplace to hoard information.
Worse, EHRs, with their cumbersome
user interfaces and onerous billing
requirements, have become a burden
to doctors and nurses, contributing
to burnout and information overload
among physicians, and degrading
patient care. “A clinician will make
roughly 4,000 keyboard clicks during a
busy 10-hour emergency-room shi,”
writes Abraham Verghese, Professor for
the Theory and Practice of Medicine at
Stanford Medicine, in the New York
Times Magazine.
“In the process, our daily progress
notes have become bloated cut-and-
paste monsters that are inaccurate
and hard to wade through.”
Although EHRs have many problems,
there are reasons to believe that
they will eventually start living up to
their promise. With some changes in
technology, regulations, and attention
to training, EHRs may soon serve
as the backbone of an information
revolution in health care, one that will
transform health care the way digital
Future of EHR
“
There are a lot
of reasons to be
optimistic that
we will be able to
have both high-
tech and high-
touch medicine.
-Lloyd B. Minor, MD
Carl and Elizabeth
Naumann Dean
Stanford University School
of Medicine

technologies are changing banking,
finance, transportation, navigation,
Internet search, retail, and other
industries. Regulations are being put in
place that will put patients in control of
their own health records and facilitate
the sharing of data among health care
organizations. Engineers are developing
artificial intelligence technology that can
“take notes” for physicians, summarize
the important points from a patient’s
record and assist in medical decision
making. Apple’s recent app for medical
information, which gives third-party
developers the ability to pull information
from health records, is expected to be
the first of many developments that
brings health care data to patients’
fingertips. In August, technology firms
including Alphabet, IBM, Amazon and
Apple pledged to “share the common
quest to unlock the potential in health
care data, to deliver better outcomes
technologies are changing banking,
finance, transportation, navigation,
Internet search, retail, and other
industries. Regulations are being put in
place that will put patients in control of
their own health records and facilitate
the sharing of data among health care
organizations. Engineers are developing
artificial intelligence technology that can
“take notes” for physicians, summarize
the important points from a patient’s
record, and assist in medical decision
making. Apple’s recent app for medical
information, which gives third-party
developers the ability to pull information
from health records, is expected to be
the first of many developments that
brings health care data to patients’
fingertips. “There are a lot of reasons
to be optimistic that we will be able to
have both high-tech and high-touch
medicine,” says Minor.
This white paper is intended to provide
a roadmap for this transformation. We
will explore the current state of the
EHR, reporting the results of a survey by
Stanford Medicine and The Harris Poll
“
A clinician will
make roughly
4,000 keyboard
clicks during a
busy 10-hour
emergency room
shi.
-Abraham Verghese, MD, MACP
Linda R. Meier and Joan F.
Lane Provostial Professor
Stanford University School
of Medicine
of physicians and their experiences and
attitudes with EHRs.
Most important, we will oer some
concrete suggestions for solving the
problems that physicians confront
today with regard to EHRs and how
the medical profession can fully
leverage the power of medical data
over the next decade.
We will distill the key ideas from a
symposium of health care industry
professionals, hosted by the Stanford
University School of Medicine on June
4, 2018, including a vision of how
EHRs could contribute positively to
health care and medicine by 2028,
how to exploit the best ideas from the
tech industry to make it happen, and
immediate and practical steps that
health care professionals can take
towards this vision.
Future of EHR

The Vision
for 2028
What would a health care
system with a fluid movement of
information and state-of-the-art
technology look like?
In an ideal world, physicians, nurses,
and other health care practitioners
would simply take care of their patients
without having to think much about
health records at all. They would devote
most of their time and attention to
interacting with the patient. Whatever
the outcome of the examination,
relevant information would flow
seamlessly to all parties necessary to
handle the patient’s progress through
the health care system—to insurance
companies, hospitals, other physicians,
and the patient.
In terms of the electronic health record
itself, this means that the EHR would be
populated with little or no eort. When
the nurse or doctor takes vital signs,
these would be automatically uploaded.
In the exam room, an automated
physician’s assistant would listen to the
interaction between doctor and patient,
and, based on the communication in
the room and verbal cues from the
clinicians, record all relevant information
in the physical exam.
The automated physician’s assistant
would also oer options for taking
action. It would use artificial intelligence
(AI) technology to synthesize medical
literature, the patient’s history, and
relevant histories of other patients
whose records would be available in
anonymized, aggregated form. When
the assistant hears a complaint from
the patient, the EHR would populate
dierent possible diagnoses for the
clinician to investigate. It would also
be sensitive to an individual patient’s
characteristics—lifestyle, medication
history, genetic makeup—and bring
all the relevant medical knowledge to
bear on what would be best treatment
options for a particular patient.
This kind of medical decision-making
support would bring Precision Health
into the doctor’s practice, with the
goal of keeping people healthy.
Knowledge would flow not only to the
clinician that is caring for a particular
patient, but also to public health oicials
interested in the population at large. We
can imagine a future where EHRs are
part of a rich, seamless data stream that
facilitates doctor-patient rapport even as
it delivers real-time diagnostic support.
Clinicians would be free to do what they
do best: use their brains and interact
with other human beings.
Future of EHR
The current reality of EHRs is less
inspiring. As a starting point, The Harris
Poll conducted a survey on behalf of
Stanford Medicine that explores the
attitudes physicians have about EHRs in
their practices. The online survey took
place between March 2 and March 27,
2018. Respondents were 521 primary
care physicians in the United States,
whose medical specialty was defined
as Family Practice, General Practice or
Internal Medicine, recruited through
the American Medical Association lists.
Results were weighted to bring gender,
region, and medical specialty into line
with actual proportions of doctors in
the country. They were licensed to
practice in the U.S. and had been using
their current EHR system for at least one
month.
When EHRs were first introduced, the
hope was that they would liberate
patient health information and
would lead to better insights and
care.
But primary care doctors are clear in
the survey and in conversation that
the opposite has happened: EHRs too
oen get in the way of better care. In the
Stanford Medicine-Harris poll, doctors
report that more than 60 percent of
their time spent on behalf of patients
is actually devoted to interacting with
EHRs. Half of oice-based primary care
physicians think using an EHR actually
detracts from their clinical eectiveness.
Writes Verghese:
“In America today, the patient in
the hospital bed is just the icon, a
placeholder for the real patient who
is not in the bed but in the computer.
That virtual entity gets all our
attention.”
Christine Sinsky, MD, Vice President of
the American Medical Association in
charge of professional satisfaction, says
that these results accurately reflect her
experience as a physician. “I’ve made
site visits to over 50 practices. I’ve given
more than 200 presentations at society
meetings, health system meetings,
grand rounds at academic medical
centers. The conversations I’ve had in
those places align with findings of the
Stanford Medicine survey,” she says. “If
anything, they underestimate the degree
of professional angst and moral distress
that physicians have experienced as
they deal with this tool.”
The angst comes when physicians have
to make trade-os between the amount
of time they spend with their patients,
the amount of time they spend creating
documentation of their encounter with
each patient, and the amount of time
they have le for families and friends.
“
If anything, they
underestimate
the degree of
professional angst
and moral distress
that physicians
have experienced
as they deal with
this tool.
-Christine Sinsky, MD
VP of Professional
Satisfaction
AMA
2018: The Current
State of Electronic
Health Care Records
Future of EHR
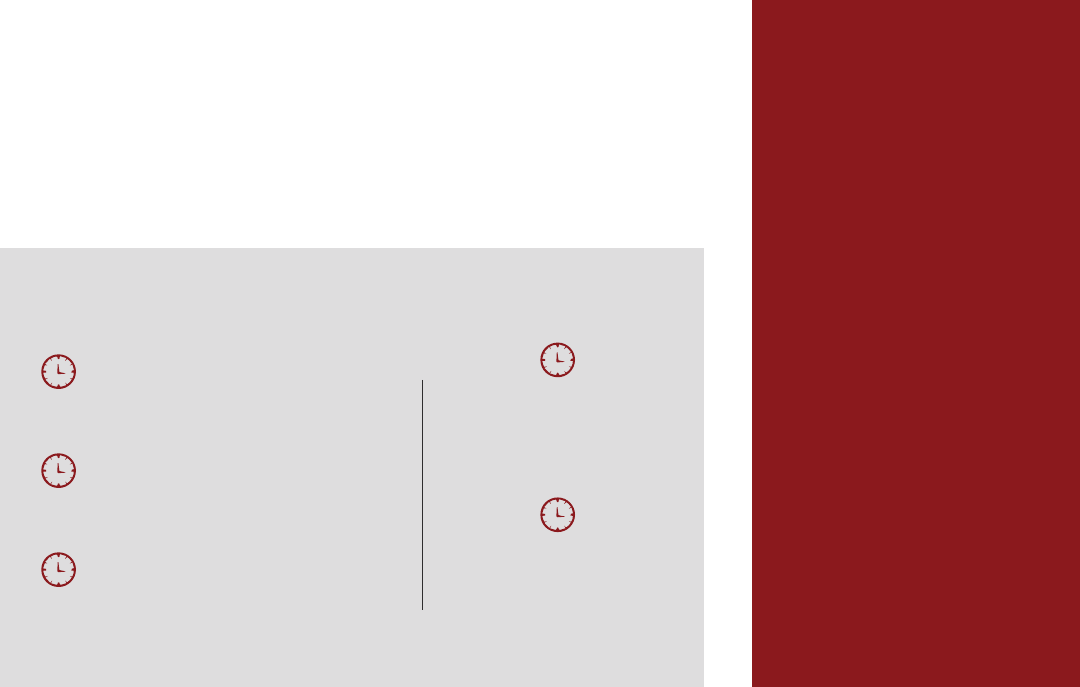
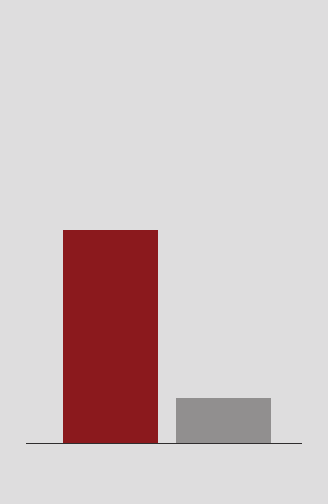
11.8 minutes
Interacting directly with a
patient during a visit
8.3 minutes
Interacting with the EHR
system during a patient visit
10.6 minutes
Interacting with the EHR
system outside of a patient visit
18.9
Total time
spent in EHR
62%
of time spent in the EHR
per patient
How Physicians Are Spending Their Time Per Patient
Source: Stanford Medicine-The Harris Poll
Physicians in their practice have to
synthesize a great deal of information,
and EHRs oen make this task more
diicult, says Sinsky. EHRs are oen
designed with dropdown menus that
increase the cognitive workload on the
physician. Doctors report anecdotally
being able to see fewer patients, having
to spend more time working, and feeling
dissatisfaction with the work they do.
Whereas previously a physician
might dictate a brief medical note,
they are now oen responsible
for the clerical work of formatting
electronic notes, which increases the
time spent on documentation.
Medicare and Medicaid reporting
requirements have made this problem
worse by requiring physicians to
document every action taken on behalf
of the patient. “As good as the EHRs
are as they exist right now, they’re not
nearly as intuitive as they should be,”
says Marc Harrison, MD, President and
CEO of Intermountain Healthcare.
“They actually can get in the way of the
patient-doctor interaction. As a nation,
we are taking our doctors and nurses
and making them into data-entry clerks.
It’s not fun, it contributes to burnout, it’s
non-value-added time.” Few physicians
see any clinical value in their EHRs. Only
8 percent cite factors related to clinical
matters, such as disease prevention
and management (3 percent), clinical
decision support (3 percent), and patient
engagement (2 percent). On the other
hand, 44 percent of physicians say the
primary value of EHRs is to serve as
digital storage.
Where do we go from here? Nearly
three-quarters of doctors in the poll
say the first order of business should
be improving the user interface of
EHRs to enhance eiciency and reduce
screen time. Half want to see data entry
shied to support sta and 38 percent
would welcome a highly accurate voice
recording technology that would act as a
scribe during patient visits.
The poll also indicated some
long-term concerns. More than 40
percent of doctors would like to see in
the next decade EHRs transformed into
a powerful tool that helps with clinical
“
They actually get
in the way of the
patient-doctor
interaction. We
are taking our
doctors and nurses
and making them
into data-entry
clerks. It’s not fun,
it contributes to
burnout, it’s non-
value-added time.
-Marc Harrison, MD
President and CEO
Intermountain Healthcare
Future of EHR
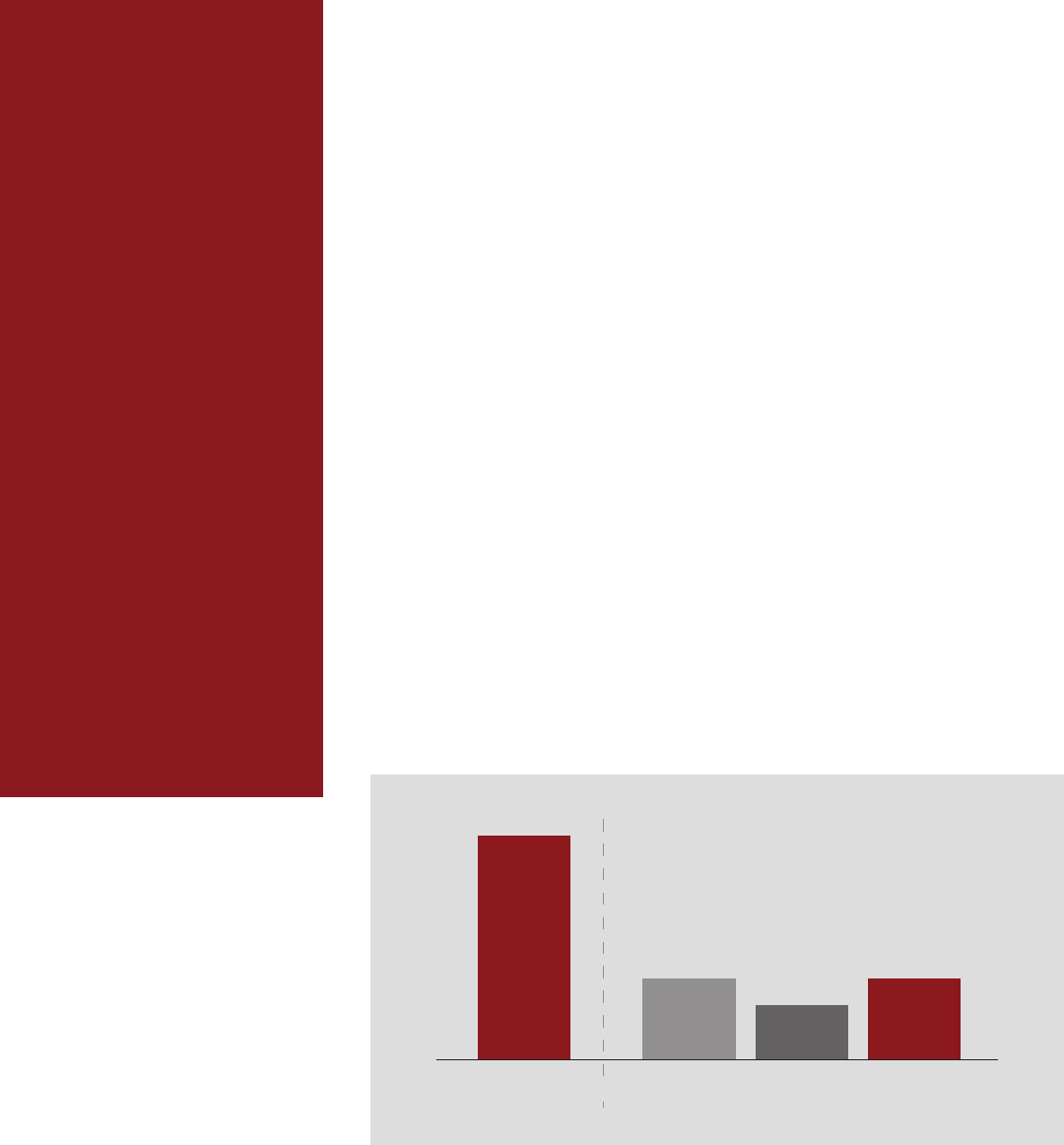
44 percent of physicians say the primary
value of the EHR is to serve as digital storage.
Only 8 percent cite factors related to
clinical matters.
TOTAL DISEASE
PREVENTION
CLINICAL
DECISION
SUPPORT
PATIENT
ENGAGEMENT
8%
3%
2%
3%
Source: Stanford Medicine-The Harris Poll
care, predictive analysis to support
disease diagnosis and prevention,
and population health management.
About a third would like to see financial
information integrated into the system
so that patients can weigh the costs of
their care options.
The top area of interest among
respondents was “interoperability”—the
need to make patient data available
easily and readily to professionals from
all parts of the health care system for the
benefit of the patient.
More than two-thirds of doctors
listed this as the No. 1 issue to fix
in the long term. To do that, we
have to have a radically dierent
health IT infrastructure—one that
promotes data sharing and is open to
developers.
The Importance of
Managing Change
Changes in technology, regulation,
and the business of health care
could transform medicine in the next
decade. In the short term, however,
physicians can take some steps to
alleviate the burden on their practices
from EHRs. Following best practices
for implementing EHRs can improve
physician satisfaction and improve
patient care. Judging from the
experience of some of the best-run
health care provider organizations,
the most practical and significant step
physicians can take is to better learn
how to use their current EHR systems.
The amount of training physicians get
in their EHRs has a big impact on their
own levels of satisfaction. Although
satisfaction is low on average among
physicians, surveys by KLAS, a health
care information-technology research
firm, show wide variation in satisfaction
levels among organizations, which
suggests that some are managing their
use of EHRs better than others. “While
less than half of physicians feel that their
EHR enables quality care, we’ve come
across a half dozen organizations where
over 75 percent of their physicians feel
that their EHR enables high-quality
care,” Taylor Davis, Executive Vice
President for Analysis and Strategy at
KLAS Enterprises, told the Stanford
Medicine symposium.
These organizations are not necessarily
the ones that have been most aggressive
at adopting the latest technology.
Instead, they emphasize teamwork
and training—and they’ve devoted
higher than average amounts of time to
training physicians to use EHRs. “Their
physicians realize that it’s a myth that
the EHR is going to be intuitive enough
to use out of the box,” said Davis. “It’s
not their technology, it’s their change
management.”
“
While less than
half of physicians
feel that their EHR
enables quality
care, we’ve come
across a half dozen
organizations
where over 75
percent of their
physicians feel that
their EHR enables
high-quality care.
-Taylor Davis
EVP, Analysis and Strategy
KLAS
Future of EHR
Short-Term EHR
Fixes
1 of 4 PCPs believe there should be
better training on how to
maximize the value of their EHR
27%
Source: Stanford Medicine-The Harris Poll
Some organizations are trying to limit
physician training for using EHRs to
an hour or two, while others put them
through two-week programs. “What’s
clear is that the organizations with the
least physician burnout are the ones
where physicians have had longer
training sessions,” says C.T. Lin, MD, Chief
Medical Oicer at University of Colorado
Health.
“And it’s not about how to use the
EHR. It’s about how we provide care,
with the EHR as one of the main
tools.”
A few years ago, Lin and his colleagues
at Colorado Health realized that many
of the physicians and nurses at its 400
clinics were dissatisfied with their EHRs.
They started an experiment, called
Sprint, in which they sent an 11-person
team to one clinic at a time to perform
custom training and development.
The goal of the Sprint team was to
address physician burnout and help
the clinic work better as a team. The
team was composed of one physician
informaticist, one nurse informaticist,
one project manager, four analysts who
can build things, and four trainers.
When the team would show up at a
clinic, physicians and administrators
would oen insist that they needed
nothing less than a complete overhaul
of the systems they use for keeping
electronic patient records. Oen,
however, their current systems already
provided much of the specific features
and functionality they needed.
“Typically, three-quarters of what they
ask for the system already does,” says
Lin. “We would say, ‘Oh, you know the 17
clicks you have to click to perform that
task? Try that button instead.’ And they
would say, ‘How long have we had one
of those?’”
The reason clinicians didn’t know
about features they needed is
because they didn’t get adequate
training at the outset, or they
weren’t brought up to speed when
new systems were rolled out or
incremental changes were made.
“
People get this
sort of empowered
feeling of like, now
that you’ve le,
we can carry on
the work because
you’ve shown us
a better way of
working. That’s the
surprising finding
out of Sprint.
-CT Lin, MD
Chief Medical Information
Oicer
UCHealth
Future of EHR
TRAINERS
ANALYSTS
PHYSICIAN
INFORMATICIST
PROJECT
MANAGER
NURSE
INFORMATICIST
Responsibilities
Sprint Teams
30%70%
Develop methods
for better
communication
Help build
things the record
systems can’t do
For this reason, each Sprint team comes
with four trainers who bring physicians
and other practitioners up to speed.
In many cases, management failed to
design the clinic’s workflow to take
advantage of the capabilities of the EHR.
About 30 percent of a Sprint team’s job
is to build things that the clinic’s current
records system doesn’t do. These can
include making up a flow sheet or a new
kind of synopsis report—anything that
a physician needs for their specialty but
for one reason or another never got. The
team generally delivers these projects
a day or two aer a physician asks for
them. “People feel like, at the end of
those two weeks, someone cares,” says
Lin.
The Sprint team also inculcates better
habits of communication among
members of clinical teams. For instance,
they introduce the practice of holding
team huddles every day. “People get this
sort of empowered feeling of like, now
that you’ve le, we can carry on the work
because you’ve shown us a better way of
working,” says Lin. “That’s the surprising
finding out of Sprint.”
Colorado Health assembled its first
Sprint team by borrowing from its
existing sta. Early on, executives
considered disbanding the team, but
its reputation had already spread to
department heads, who were eager
to know when they would be seeing a
Sprint team in their clinic. Two years
aer the experiment was started,
Colorado Health put together a second
team. The SWAT-team approach has
its drawbacks. It takes resources and
suers from a lack of scalability. Even
with two teams and a rapid-fire ethos, it
will take 10 years for Colorado Health’s
two teams to work through 400 clinics.
An alternative, says Lin, is to be strategic
about which pain points to target. If
an organization can’t aord to create a
SWAT team of 11 people for two-week
stints, it may be possible to construct
a team of, say, three people who can
accomplish half as much. “If the New
York Times publishes a béarnaise sauce
recipe that’s not in your fridge, you
have to work with what you’ve got,”
says Lin. “Can I get to 80 percent of
the deliciousness using what I already
have?”
Other health care organizations have
used up-front training to achieve
better physician satisfaction.
NorthShore University HealthSystem
created an onboarding program for
physicians that called for four to six
hours of training on their Epic EHR
systems. Within two weeks, physicians
also completed three full days of one-
on-one training by clinical trainers
with backgrounds primarily in nursing.
The amount of required training time
is adjusted if physicians can show
proficiency with an EHR and completed
their residency in an environment that
uses Epic. Training time can also be
extended as needed.
NorthShore’s clinical trainers typically
meet recently hired physicians at the
physician’s oice one hour prior to the
first scheduled patient. The trainers
get the physicians set up in the system
and answer questions. Trainers stay
the entire day to provide one-on-one
support. This process is repeated on
the second day. The trainer returns the
following week to ensure that there are
no remaining concerns about how to
use the EHR.
Greater Hudson Valley Health System,
a community hospital, got good results
by enlisting physicians to help them
prioritize development tasks. This
allowed them to reduce the time to
implement changes requested by
physicians to within two days. Greater
Hudson Valley also established a
governance process that gave the
organization some nimbleness in
responding to health crises, such as a
measles outbreak in 2018. This idea was
to allow for changes in workflows in
response to a crisis without introducing
confusion. Their solution was to have
analysts meet regularly with clinicians
to determine the top five issues
they want action on. The hospital’s
information technology sta also began
Future of EHR
to use Epic’s analytics tools to measure
productivity, to find the best workflow
that increases the quality of patient
care. During the measles outbreak,
IT met with the hospital’s lawyers,
quality-control personnel, nurses, and
infectious disease experts to determine
how best to modify EHRs to make them
more useful in managing the crisis.
The changes took a matter of hours to
implement.
Central to the success of Great Hudson
Valley’s program is making analytics
data available to physicians. Since the
clinicians helped narrow down the list
of priorities, it is important that they are
able to access data they need to make
appropriate decisions.
For physicians and health care
organizations that handle Medicare
and Medicaid patients, the federal
government is beginning to move
away from some of its more onerous
requirements for documenting the
patient-doctor interaction.
Its recent “Patients Over Paperwork”
initiative, announced in June 2018,
would consolidate some Medicare fee
structures for outpatient
visits, reduce clerical tasks associated
with coding and billing administration,
and allow doctors and other
practitioners to focus on documented
changes since the patient’s last visit
rather than re-documenting information.
The Centers for Medicare and Medicaid
Services (CMS) estimates that the new
regulations would save nearly 30,000
hours spent on billing administration.
If these changes are adopted, they
might relieve some of the burden on
physicians in the next few years.
Ineiciencies in Billing
and Reimbursement
Physicians and patients alike have their
favorite anecdotes about the problems
of the U.S. health care system. Many
of these stories center on the process
of billing and reimbursement. Terry
Gilliland, MD, Senior Vice President and
Chief Health Oicer at Blue Shield of
California, told the Stanford Medicine
symposium that overhead for billing
transactions accounts for 6 percent of
a payer’s costs. One practice reported
that it takes a trained registered nurse
45 minutes on average to get insurance
pre-authorization for a CT scan. Another
practice reported that, over the course
of dealing with all of their dierent
payers and care organizations, they are
required to fill out 200 dierent forms.
In general, health care billing in the U.S.
is characterized by a pervasive fear of
technology and ineiciency.
“This is an extremely fragmented
manual process that is not
benefitting many people,” says
Gilliland.
One problem is a lack of automation
of manual processes. About a third
of physician practices insist on doing
business with paper forms and fax
machines. A physician’s oice might fill
out a claims form on paper and fax it
to the payer, who would pay someone
to transcribe it into their system. Then
the payer will identify information that
is missing in the form but is needed
to process a claim. The form then gets
faxed back to the doctor’s oice, which
addends it and faxes it back. The payer
then has to pay someone to transcribe
the information into the system. These
kinds of ineiciencies drive up the cost
of transactions.
Future of EHR
Ineiciencies
In Billing and
Reimbursement
One practice reports it takes a
trained nurse 45 minutes, on
average, to get insurance
pre-authorization for a CT scan.
Another practice reports that,
over the course of dealing with all
of their dierent payers and care
organizations, they are required
to fill out 200 dierent forms.

Despite the rapid adoption of EHRs,
there has not been a commensurate
reduction in fragmentation and
automation in the realm of billing.
This is ironic considering that the
conventional wisdom among physicians
is that billing is the primary purpose
of EHRs in the first place. Standards
for Application Programming
Interfaces (APIs), which allow soware
from dierent devices to exchange
information securely and eiciently,
may help alleviate some ineiciencies
in billing. (We’ll discuss APIs further
below.) For instance, an API may give a
payer access directly to the information
it needs to process a claim, rather
than having to exchange faxes with
the doctor’s oice. The change in
recent years from transaction-oriented
reimbursement schemes, in which
health care providers are paid for,
and have to document, each act they
perform, to those that emphasize the
value of health care services to the
patient, has lowered the volume of
forms and documentation somewhat.
Fewer practices are required to
document things that they’ve done to
get reimbursement.
Physicians: Junk the fax machine.
Every doctor’s oice ought to
embrace electronic communications.
“For the 30 to 40 percent of American
practices that are unwilling to give
up the fax machine and are unwilling
to receive electronic payments,
perhaps there has to be a culture
shi,” Gilliland told symposium
attendees. Federal and private payers
may be able to help in this regard by
providing incentives. Even simple
changes such as physician practices
shiing to a payer’s portal website,
rather than insisting on using faxes
and paper payments, would create
significant eiciencies.
Physicians must start accepting
electronic payments. Many doctors’
oices are reluctant to allow payers
to transfer funds electronically for
fear that they would also be able to
make withdrawals.
Payers need to support physician
practices. Providing in-kind support
to providers in exchange for sharing
clinical and claims information would
help practices adopt technology.
For instance, payers could provide a
dashboard back to providers so that
they can get analytical insights about
their utilization and costs. This would
have the added benefit of helping
them make the transition to value-
based billing.
Create common standards across
payers. If health care insurers and
other payers agree on a common
set of data and formats, they would
greatly reduce the bureaucratic
burden on small practices who now
must fill out so many dierent forms.
Streamline pre-authorization.
Decreasing the hassle and time to
process claim pre-authorizations
would reduce ineiciencies and
2.
3.
Future of EHR
4.
Gilliland identified some
practical, short-term steps
to help streamline billing:
1.
5.

enhance patient care. Physician oices
should get instant feedback on pre-
authorizations. It should not take 45
minutes of a nurse’s time on the phone
to get authorization.
Artificial Intelligence
Can Improve the Doctor-
Patient Interaction
Artificial intelligence holds great promise
for alleviating some of the burden on
physicians of working with electronic
health records and freeing the physician
to focus on the patient during an
examination rather than on filling
out forms.
AI can potentially help physicians
get up to speed on a patient’s clinical
history, take notes and document the
visit with the patient, and support
medical decisions about what to do
next.
A clinician, upon walking into an
examination room, needs knowledge
about the patient’s background
and history. The EHR as currently
implemented in many organizations
is not designed to impart knowledge.
It contains a great deal of information,
but it can be diicult for physicians to
locate specific information needed for
informed decision-making. The quality
of much of the information is poor—
much of it is put there for non-clinical
purposes, such as documenting patient-
doctor interactions with billing codes to
satisfy regulators and insurers. “If you
could document just what you need
to take care of the patient, the volume
of notes in an EHR would shrink by 70
percent,” says Paul Tang, Vice President
and Chief Health Transformation Oicer
at IBM and a symposium participant.
All that extra information obscures
whatever useful information the EHR
contains, and makes the doctor’s job
harder.
Reading a patient’s record in the EHR
and gleaning insight from it is a high-
level cognitive task. “You wouldn’t ask
a medical student to do it or you’d get
back a ton of stu,” says Tang. He and
others are working on natural language
processing technologies that can read
“
If you could
document just
what you need to
take care of the
patient, the volume
of notes in an EHR
would shrink by 70
percent.
-Paul Tang, MD, MS
Chief Health Transformation
Oicer
IBM Watson Health
Future of EHR
Top Value Propositions
of Funded AI/ML Digital
Health Companies
(Total Funding Raised)
CLINICAL
WORKFLOW
HEALTH
BENEFITS
ADMIN
$514.8M
$469.5M
the text and data on the record and use
machine learning algorithms to choose
what information is relevant. The act
of writing a note is also a high-level
cognitive task: it requires a synthesis of
the clinician’s experience in the exam
room, which includes not only the
words that are spoken in conversation
but also non-verbal cues and medical
judgements in the physician’s head.
Clinicians used to write succinct notes
on paper records. Now they too oen
use the copy-and-paste function on their
computers to add excessive amounts of
information, which makes it that much
harder to find what’s relevant.
Source: Rock Health
Studies show that physicians who use
medical assistants to act as “digital
scribes” and record the content of the
patient-doctor interaction show far more
satisfaction and lower rates of burnout.
University of Colorado Health
experimented with increasing the ratio
of Medical Assistants (MAs) to physicians,
from 0.4 MAs per physician to nearly two.
Before the physician enters the room, an
MA spends 20 minutes talking with the
patient, updating the medical records
and handling minor medical issues,
such as vaccines and screenings. When
the physician walks in, the MA stays in
the room, acting as a scribe during the
exam. They found that over the course
of a year, this approach went a long
way to relieving physician burnout: the
metric they use to measure physician
burnout declined from 55 percent to 14
percent. Assigning two people for each
physician to act as scribe may not be a
cost-eective solution, however.
AI researchers are working on
automating the job of scribe. Google
and Stanford Medicine have been
working for more than a year on
a digital scribe project that would
listen to the dialogue in a patient
visit and take notes.
The idea is not merely to take a
transcription, but rather to knit the
dialogue into a narrative. In the study,
each doctor wears a microphone to
capture conversations with patients,
which are used to train machine-
learning algorithms in getting the gist of
a doctor-patient interaction. The goal is
to train the algorithm to generate a pithy
progress note.
Google researchers say that
its scribe can capture complex
conversations typical of a patient-
doctor conference even when family
members and other practitioners are
present in a noisy environment.
AI can also potentially assist doctors
in making medical decisions at the
end of a patient visit. For instance, if a
patient who is already on medication for
hypertension comes into the doctor’s
oice with high blood pressure, what
should the doctor do: increase the
dosage or try another drug altogether,
and if so, which one? Doctors oen have
to make these kinds of decisions with
incomplete information on the patient
or on population studies of the drug’s
eicacy. The physician then needs to
do considerable research to determine
the best medical course of action. An
AI assistant that could take in relevant
information about the patient in the
EHR and combine it with a review of the
medical literature could save the doctor
a great deal of time.
In a study recently published in Nature
Digital Medicine, researchers at the
University of California, San Francisco,
University of Chicago Medicine, Stanford
Medicine, and Google used an advanced
algorithm to predict unexpected
readmissions, long hospital stays, and
in-hospital deaths among 216,000 adult
patients using data from their EHRs. The
study suggests that machine-learning
algorithms can make sense of messy
electronic health record data, including
unstructured clinical notes, errors in
labels, and large numbers of input
variables, to make predictions about
patient health. Another study at Stanford
Medicine uses algorithms to si through
large databases, including electronic
health records, to detect patients who
likely have a certain genetic condition
that can lead to a fatal heart attack at a
premature age.
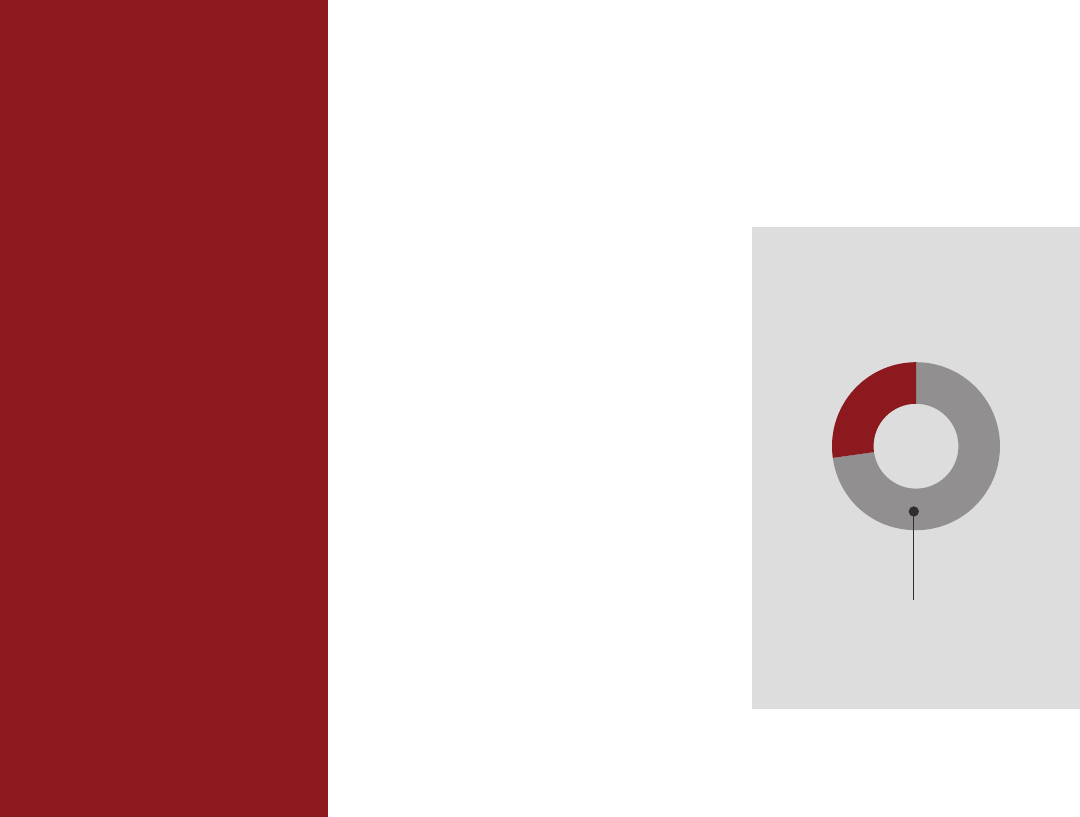
A combination of AI and information
CHART
55%
14%
Over the course of one year there was a
decrease in physician burnout at the
University of Colorado Health due to the
addition of more medical assistants to help
physicians with note entry.
Future of EHR
Physician Burnout
OVER ONE YEAR
BEFORE
AFTER
from patient records could also advance
the ball on Precision Health.
Based on an individual’s
characteristics, AI could draw
on sources of big data to
oer personalized treatment
recommendations, based on:
The patient’s past medical history
Genomic information
The way the patient metabolizes
certain drugs
Relevant medical literature
Similar patients in the population
Environmental and social factors
Intermountain Healthcare, for instance,
is studying the clinical and economic
implications of using genomics in the
treatment of behavioral health. It is
currently using genomics in the care of
people with depression—specifically
to determine which antidepressants at
which doses will be most eective for a
patient based on their particular drug
metabolism. The company is planning
similar studies for anti-psychotic and
bipolar patients. Combining genomics
with machine learning could be a
powerful predictive tool.
An AI-based decision support system
for individual doctors could serve as
a window to data from many other
sources, and could be a major tool in
preventive and personalized health.
An App-Based Ecosystem
Can Put Patients at the
Center
Perhaps the biggest disappointment
of EHRs is that they are still to a large
degree static. Although they store data
electronically, that data is still trapped
within the institutions that gather it.
The next step in the digitization of
health care, symposium participants
agreed, is to free up this information
in ways that enhance patient health
while protecting privacy. The goal is to
leverage data in the EHR to enhance
patient care. This should happen in an
information marketplace that empowers
patients and health care providers to
configure their own EHR experiences
and workflows.
Harris Poll respondents overwhelmingly
called for greater interoperability of data
in EHRs. In other words, the information
in EHRs should pass seamlessly
among health care organizations and
patients. This includes all the ways
patient records are currently exchanged
among providers and payers and
patients, but also new ways that would
enhance patient care. For instance,
aggregate data from EHRs would help
in determining what medical resources
should be deployed strategically across
a population to help manage risks.
“When predictive models are enriched
by clinical data, they are richer and more
accurate,” says Rishi Sikka, MD, President
of System Enterprises, Sutter Health.
If physicians can make more accurate
predictions, they can intervene in
meaningful ways to prevent illness.
Free movement of data would also
improve patient health by eliminating
unnecessary tests. Whenever a blood
test is done because the records of
a previous test were unavailable, or
“
When predictive
models are enriched
by clinical data, they
are richer and more
accurate.
-Rishi Sikka, MD
President, System Enterprises
Sutter Health
Future of EHR
whenever an x-ray is taken because
a previous image was not readily
available, patients are exposed to undue
risk.
A lack of available information also
1.
2.
3.
4.
5.
6.
makes it more diicult to make good
medical decisions. Physicians are oen
in the dark about what their patients do
aer they leave the examination room.
A doctor may not know, for instance,
whether a patient with diabetes has
filled a prescription for insulin, even
though this information is critical to the
patient’s health. “Typically, information
does not go back from pharmacy to
doctor,” says Roy Beveridge, Chief
Medical Oicer of Humana. “There’s no
feedback loop. This is simple to do if
there’s connectivity,” says Beveridge. “It’s
why interoperability is so important.”
Even organizations that have a greater
than usual need to exchange
information struggle with
interoperability. A survey published
in July 2018 in JAMIA of 68 hospitals
found that even those organizations
that frequently shared patients didn’t
do very well at exchanging records. Of
63 pairs of hospitals studied, 23 percent
reported worse information sharing
between the hospitals with which they
regularly share patients, with 17 percent
reporting better sharing and 48 percent
indicating no dierence. “New policy
eorts, particularly those emerging from
the 21st Century Cures Act, need to
explicitly pursue strategies that ensure
that [highest shared patient] providers
engage in exchange with each other,”
conclude authors Julia Adler-Milstein of
University of California, San Francisco,
who spoke at the Stanford Medicine
symposium, and Jordan Everson of
Vanderbilt.
One obstacle to the free flow of
information is perverse incentives in
the businesses that deal with EHR
systems. Health care organizations
that gather data about patients have
a proprietary interest in that data—
they want it to flow only if they are
compensated for it. “Unless there’s a
free exchange of data, your hospital
believes that its data is valuable to
them, and they’re not releasing it to the
“
This is simple
to do if there’s
connectivity,
it’s why
interoperability
is so important.
-Roy Beveridge, MD
Chief Medical Oicer
Humana
Future of EHR
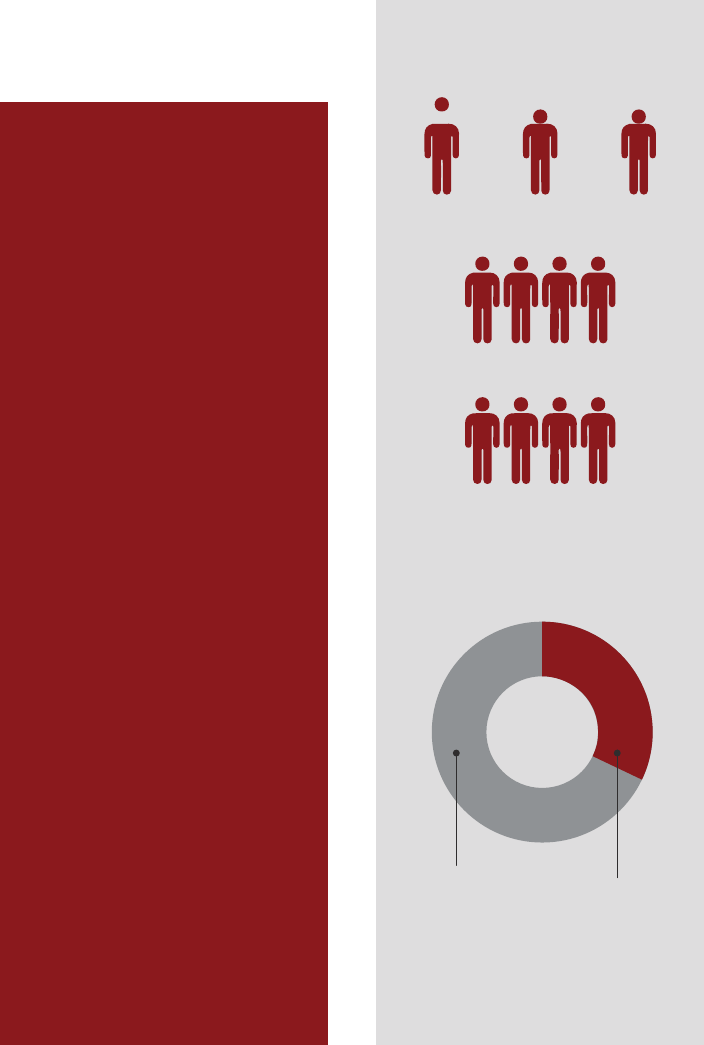
Reported worse
information sharing
Reported better
information sharing
Reported no dierence in
the information sharing
23% 17% 48%
Out of 63 Pairs of Hospitals Studied That
Regularly Share Patients
Source: Journal of the American Medical Informatics Association

ophthalmologist or the pharmacy,” says
Beveridge.
“If no one is sharing information,
this simple feedback loop doesn’t
occur, because everyone’s trying to
maximize their little bit of money.”
Congress acted in 2016, with the passage
of the 21st Century Cures Act, to fix the
lack of interoperability by authorizing
HHS to investigate cases in which patient
information is not shared and imposing
penalties. “It didn’t escape Congress
that some of this information wasn’t
being shared for a variety of reasons and
that people didn’t have health care on
their smartphones,” says Don Rucker,
MD, the National Coordinator for Health
Information Technology at the Oice of
the National Coordinator for Health IT,
part of the U.S. Department of Health
and Human Services (HHS). Rucker’s
oice is currently working to promulgate
rules that flesh out the provisions of
the Act by defining permissible types of
information blocking—instances when a
business can legally refrain from sharing
information—and establishing rules for
open APIs. “We believe those rules will
be powerful,” says Rucker.
Another obstacle is concern over privacy.
Currently the practice of handling
patient medical records is governed
by a combination of state rules and
the Health Insurance Portability and
Accountability Act of 1996, or HIPAA.
Devised in the early days of the AIDS
crisis to ensure the privacy of medical
diagnoses, HIPAA forbids dissemination
of patient data without the permission
of the patient except under specific
exceptions, such as some circumstances
in which health care providers need
to exchange data about patients they
have in common. Since some state laws
are more restrictive, some people are
hesitant to exchange data even when
they are allowed to.
Health care organizations tend to have
an overly-restrictive interpretation of
HIPAA rules, says Lucia Savage, Chief
Privacy and Regulatory Oicer at Omada
Health and a former Chief Privacy Oicer
at the Oice of the National Coordinator
“
Future of EHR
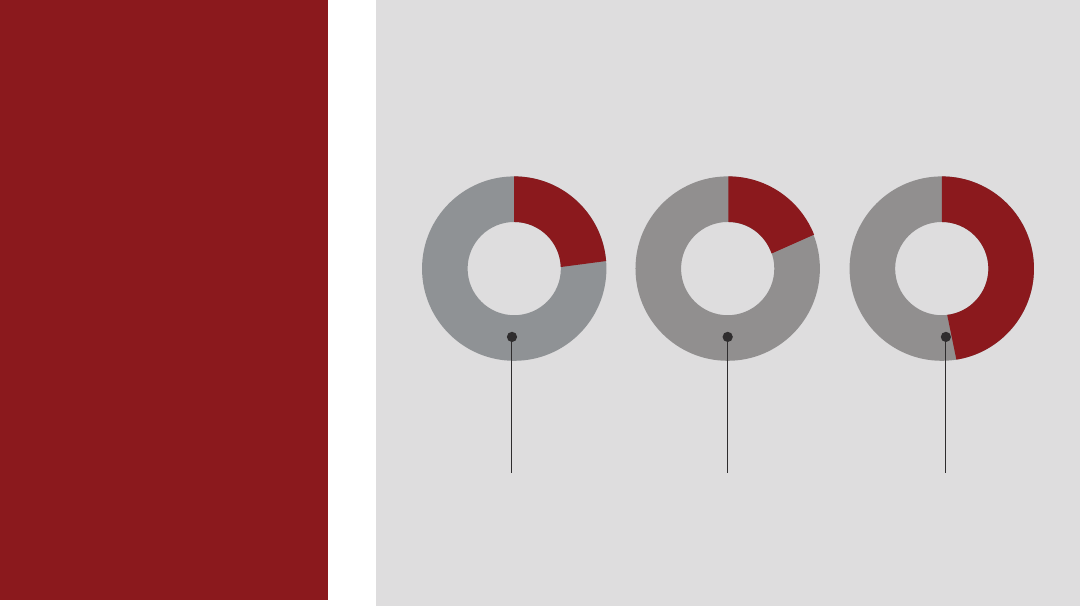
Long-Term EHR
Developments Physicians Want
Integrating financial information
into the EHR to help patients
understand the costs of their
care options
32%
Solving interoperability
(system-wide information
sharing) deficiencies
through various strategies
67%
Improving predictive analytics
to support disease diagnosis,
prevention, and population
health management
43%
It didn’t escape
Congress that
some of this
information wasn’t
being shared for a
variety of reasons
and that people
didn’t have health
care on their
smartphones.”
- Don Rucker, MD
The National Coordinator
for Health Information
Technology
ONC
Source: Stanford Medicine-The Harris Poll

of the more than 4,000 or so hospitals in
the U.S. The hope is that this situation
will improve once patients demand that
their health data is readily available, and
more institutions join the trend.
Demand from the patient user is
crucial to overcoming many of the
barriers that now stand in the way of
interoperability.
The foundation of an app-based health
care world would be the EHR. It would
be the basic repository of data about the
patient, and the patient would control
that data by granting permissions,
for Health Information Technology, in
HHS. Patients and executives are skittish
about privacy in the wake of revelations
about NSA surveillance and Facebook’s
sale of user data. An overly-restrictive
view of patient privacy when it comes to
medical records has hampered eorts to
make the data available in useful ways.
Participants at the Stanford Medicine
symposium were overwhelmingly of
the opinion that the risk of not sharing
data outweigh the risks to privacy. Says
Savage: “The best way to secure a health
record is to print it out on paper, stick it
in a box, and cover it with cement. But
then it’s of no use at all.”
A lack of standards for EHRs has also
held back progress in making data
freely available. EHRs oen contain a
mixture of formatted data and free text,
and standards vary widely from one
IT provider to the next. And they are
not interoperable with one another—
sometimes even within the same health
care organization.
In an eort to free up medical data, the
non-profit group Health Level Seven
International draed a standard called
FHIR, for Fast Healthcare Interoperability
Resources, that specifies how health
care apps can share data. HHS gave EHR
developers until January 2017 to create
FHIR-based open-specification APIs.
The Centers for Medicare and Medicaid
Services, a part of HHS, gave health
care organizations until January 2019
to provide data when a patient requests
it via a FHIR-based app. This means, in
eect, that data must be delivered when
a patient’s app requests it, so long as the
app is authentic and secure.
A year and a half later, the app
revolution hasn’t yet arrived. Resistance
from the medical community to new
technology is one factor. Privacy
concerns are another.
“People were worried that the app
would be a fraudulent app or that
identity credentials presented by the
app would be stolen,” says Savage.
“Tons of work has been done with
the medical professional to try to get
them used to this idea that in fact it’s a
completely legitimate exercise, legally
and technologically, for an individual
to give their credentials to an app that’s
acting on their behalf then for the app to
do the work of fetching.”
Many health care technology experts
believe that app-based medicine will
eventually break the logjam that is
keeping medical data from flowing
freely. Apple’s recent upgrade to its
Health app allows users to download
information from participating health
care providers onto their iPhones. At
the moment, only three or four dozen
institutions participate—a small fraction
“
Future of EHR
The best way to
secure a health
record is to print
it out on paper,
stick it in a box,
and cover it with
cement. But then
it’s of no use at all.
- Lucia Savage
Chief Privacy and Regulatory
Oicer
Omada Health, Inc.
through their acceptance of the terms
and conditions of the app, in accordance
with HIPAA and other regulations.
In a way, the EHR itself is a collection
of health care components, oen
integrated via APIs that standardize
how each one communicates with the
others. Thus, in the anticipated app-
based economy, those APIs would be
extended, using industry-accepted
security protocols, to encompass
information that patients, physicians,
and care teams could repurpose in
ways that are meaningful and useful.
It would also go a long way to solving
the interoperability problem, provided
those protocols are openly and easily
available, as is required in the Cures
Act. The power of an open API is that
it can be used to fetch information
without having to have nurses calling
insurance companies and assistants
sending faxes. The app itself contains
all the permissions and contractual
agreements required to carry out a
transaction, so there’s no checking
or double-checking involved. “It’s the
dierence between a dumb pipe and a
smart pipe,” says Aneesh Chopra, who
served as Chief Technology Oicer in
the Obama White House. “An API is a
smart pipe. It’s designed with all the
agreements built into it. It gives an app
developer the ability to get data quickly
in accordance with certain rules.” And
the app/API interaction leaves an audit
trail.
Patients, doctors, and health care
industry professionals could glean
insight from an ecosystem of health care
apps that interprets data, combines
data from dierent sources, and
communicates it to relevant parties—
patients, doctors, and health care
industry professionals. Patients could
use their smartphones to assemble their
own ecosystem of apps that meet their
own needs for health information, the
same way they’d use apps for checking
accounts or to apply for a mortgage or to
call an Uber.
The Veterans Health Administration is
trying to build such an ecosystem for its
9 million veterans and families. The VA,
which provides care at 1,240 facilities
globally, has made interoperability
a priority in its $10 billion plans
to modernize its EHR system. It is
partnering with vendors and other
health systems to ensure that its EHR
system will be 100-percent interoperable
across vendor EHRs and would
leverage APIs to create a developer-
friendly environment to nurture app
development.
About a dozen groups have signed
an industry pledge to support this
eort.
If each patient had a universe of health
care apps to pick and choose from, it
would help to democratize medical data,
Future of EHR
the way ATMs democratized banking.
From an information technology
standpoint, the challenge to medicine is
greater than it was for banking. Health
care data is inherently more complicated
than account balances and mortgage
payments. Medicine has had barely a
decade to wrestle with this particular
information challenge. The next decade
promises to be an eventful one.
For Medical Practices:
Invest in adequate EHR training when
onboarding physicians and bring
them up to speed when incremental
changes are made;
Enlist physicians to help prioritize
EHR development tasks and to
design clinical workflows that take
advantage of EHR capabilities (e.g.,
the Sprint team model);
Tailor the size and makeup of
physician development teams, taking
into account the clinical resources
available;
Deliver EHR development projects
soon aer physicians ask for them;
Establish an EHR governance process
that gives the clinical organization
nimbleness in responding to health
emergencies and crisis scenarios;
Make analytics data available to
physicians—presented in a way that
is intuitive at the point of care;
Shi non-essential EHR data entry
to ancillary sta. In the near term,
consider increasing the number of
medical assistants to act as “digital
scribes” (though this option is
expensive). In the long term, seek
automated solutions to eliminate
manual EHR documentation;
Re-evaluate your organization’s
interpretation of privacy rules;
Create opportunities for patients
to digitally maintain their records
(providing family history, medical
history, medications, health
monitoring data, etc.);
Junk the fax machine (if you still
have one) and embrace electronic
communications;
Start accepting electronic payments,
if you don’t already.
For Payers:
EHRs are a reflection of the current
fee-for-service payment paradigm.
Commit to value-based care
and provide adequate support
to physicians under this model,
including greater reimbursement for
preventive care services and the use
of digital health to engage patients;
Create common standards for billing
and quality reporting across payers;
Streamline pre-authorization
procedures;
Make claims data more accessible to
physicians to enable a longitudinal
view of their patients.
For Regulators:
Airm commitment to value-based
care and moving away from requiring
literal documentation of patient-
doctor interactions;
Create more flexibility around who
needs to enter data into the EHR,
as many tasks do not require the
expertise of a highly trained clinician;
Clarify information-blocking rules to
encourage open APIs and eliminate
perverse incentives to hoard
information.
A Summary
of Action Points
Future of EHR

For Technologists:
Clarify definitions of interoperability—
in collaboration with other
stakeholder groups—and adopt
common technical standards to
support them;
Develop systems and product
updates in partnership with your
end users—less than half of U.S.
physicians believe EHR developers
are responsive to their feedback;
Embrace open APIs and nurture a
community of developers to enable
an app-based ecosystem that puts
the patient in control;
Develop and market an ecosystem of
third-party apps that put patients in
control of their own health data;
Focus on eliminating the manual
entry of data into the EHR by
recruiting AI, natural language
processing, and other emerging
technologies;
Develop AI to increase the intelligence
of clinical information systems,
enabling them to:
Synthesize relevant information
in the EHR before each patient
encounter and present the
physician with a pithy summary;
Combine patient complaint
information with EHR databases
and the latest medical literature to
support medical decision making;
Deliver current and contextualized
information to each member of
a patient care team (i.e., enable
intelligent “care traic control”).
1.
2.
3.
Future of EHR
CHANGE OR ADAPT IN RESPONSE
TO USER FEEDBACK
Importance of vs. Satisfaction
with EHR Abilities
91%
Importance
44%
Satisfied
Source: Stanford Medicine-The Harris Poll

I
med.stanford.edu/ehr/whitepaper
